Catalogue Search | MBRL
نتائج البحث
MBRLSearchResults

وجه الفتاة! هناك خطأ ما.
أثناء محاولة إضافة العنوان إلى الرف ، حدث خطأ ما :( يرجى إعادة المحاولة لاحقًا!
-
الضبطالضبط
-
مُحَكَّمةمُحَكَّمة
-
نوع العنصرنوع العنصر
-
لديه النص الكامللديه النص الكامل
-
السنةمن:-إلى:
-
المزيد من المرشحاتالمزيد من المرشحاتالموضوعالناشرالمصدراللغةمكان النشرالمؤلفين
منجز
مرشحات
إعادة تعيين
120,264
نتائج ل
"Liver cancer"
صنف حسب:
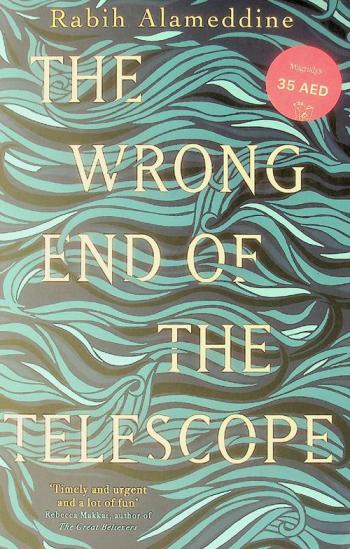
The wrong end of the telescope
Mina Simpson, a Lebanese doctor, arrives at the infamous Moria refugee camp on Lesbos, Greece, after being urgently summoned for help by her friend who runs an NGO there. Alienated from her family except for her beloved brother, Mina has avoided being so close to her homeland for decades. But with a week off work and apart from her wife of thirty years, Mina hopes to accomplish something meaningful, among the abundance of Western volunteers who pose for selfies with beached dinghies and the camp's children. Soon, a boat crosses bringing Sumaiya, a fiercely resolute Syrian matriarch with terminal liver cancer. Determined to protect her children and husband at all costs, Sumaiya refuses to alert her family to her diagnosis. Bonded together by Sumaiya's secret, a deep connection sparks between the two women, and as Mina prepares a course of treatment with the limited resources on hand, she confronts the circumstances of the migrants' displacement, as well as her own constraints in helping them.
RNA-Seq profiling of circular RNAs in human colorectal Cancer liver metastasis and the potential biomarkers
2019
In this study, the secondary sequencing was used to profile circRNA expression in the tissue samples from three CRC patients with liver metastasis and three matched CRC patients. After verified some candidates in another 40 CRC and CRC-m samples by qRT-PCR, we further demonstrated that circRNA_0001178 and circRNA_0000826 were significantly upregulated in CRC-m tissues, and both of them had the potential for diagnosing liver metastases from colorectal cancer. Finally, the networks of circRNA-miRNA-mRNA base on these two circRNAs were constructed respectively. This study showed that differentially expressed circRNAs were existed between the tissue samples from colorectal cancer patients with and without liver metastasis. And also suggested that circRNA_0001178 and circRNA_0000826 may serve as a potential diagnostic biomarker for liver metastases from colorectal cancer.
Journal Article
CD90+ liver cancer cells modulate endothelial cell phenotype through the release of exosomes containing H19 lncRNA
بواسطة
Buccheri, Simona
,
Conigliaro, Alice
,
Tripodi, Marco
في
Analysis
,
Cancer cells
,
Cell Adhesion
2015
CD90+ liver cancer cells have been described as cancer stem-cell-like (CSC), displaying aggressive and metastatic phenotype. Using two different in vitro models, already described as CD90+ liver cancer stem cells, our aim was to study their interaction with endothelial cells mediated by the release of exosomes.
Exosomes were isolated and characterized from both liver CD90+ cells and hepatoma cell lines. Endothelial cells were treated with exosomes, as well as transfected with a plasmid containing the full length sequence of the long non-coding RNA (lncRNA) H19. Molecular and functional analyses were done to characterize the endothelial phenotype after treatments.
Exosomes released by CD90+ cancer cells, but not by parental hepatoma cells, modulated endothelial cells, promoting angiogenic phenotype and cell-to-cell adhesion. LncRNA profiling revealed that CD90+ cells were enriched in lncRNA H19, and released this through exosomes. Experiments of gain and loss of function of H19 showed that this LncRNA plays an important role in the exosome-mediated phenotype of endothelial cells.
Our data indicate a new exosome-mediated mechanism by which CSC-like CD90+ cells could influence their tumor microenvironment by promoting angiogenesis. Moreover, we suggest the lncRNA H19 as a putative therapeutic target in hepatocellular carcinoma.
Journal Article
Current Approaches in Hepatoblastoma—New Biological Insights to Inform Therapy
2022
Purpose of Review
As the most common pediatric primary liver cancer with rising incidence, hepatoblastoma remains challenging to treat. Here, we review the current understanding of the biology of hepatoblastoma and discuss how recent advances may lead to new treatment modalities.
Recent Findings
Standard chemotherapy regimens including cisplatin, in addition to surgery, have led to high cure rates among patients with low stage hepatoblastoma; however, metastatic and relapsed disease continue to have poor outcomes. Recent genomics and functional studies in cell lines and mouse models have established a central role for the Wnt/β-catenin pathway in tumorigenesis. Targeted agents and immunotherapy approaches are emerging as potential treatment avenues.
Summary
With recent gains in knowledge of the genomic and transcriptomic landscape of hepatoblastoma, new therapeutic mechanisms can now be explored to improve outcomes for metastatic and relapsed hepatoblastoma and to reduce the toxicity of current treatments.
Journal Article
Towards an international pediatric liver tumor consensus classification: proceedings of the Los Angeles COG liver tumors symposium
بواسطة
Finegold, Milton J
,
Meyers, Rebecka
,
Katzenstein, Howard
في
Algorithms
,
Child
,
Classification
2014
Liver tumors are rare in children, and their diagnoses may be challenging particularly because of the lack of a current consensus classification system. Systematic central histopathological review of these tumors performed as part of the pediatric collaborative therapeutic protocols has allowed the identification of histologic subtypes with distinct clinical associations. As a result, histopathology has been incorporated within the Children's Oncology Group (COG) protocols, and only in the United States, as a risk-stratification parameter and for patient management. Therefore, the COG Liver Tumor Committee sponsored an International Pathology Symposium in March 2011 to discuss the histopathology and classification of pediatric liver tumors, and hepatoblastoma in particular, and work towards an International Pediatric Liver Tumors Consensus Classification that would be required for international collaborative projects. Twenty-two pathologists and experts in pediatric liver tumors, including those serving as central reviewers for the COG, European Société Internationale d'Oncologie Pédiatrique, Gesellschaft für Pädiatrische Onkologie und Hämatologie, and Japanese Study Group for Pediatric Liver Tumors protocols, as well as pediatric oncologists and surgeons specialized in this field, reviewed more than 50 pediatric liver tumor cases and discussed classic and newly reported entities, as well as criteria for their classification. This symposium represented the first collaborative step to develop a classification that may lead to a common treatment-stratification system incorporating tumor histopathology. A standardized, clinically meaningful classification will also be necessary to allow the integration of new biological parameters and to move towards clinical algorithms based on patient characteristics and tumor genetics, which should improve future patient management and outcome.
Journal Article
Dysregulated long noncoding RNAs (lncRNAs) in hepatocellular carcinoma: implications for tumorigenesis, disease progression, and liver cancer stem cells
بواسطة
Hebbard, Lionel
,
Latchoumanin, Olivier
,
Huo, Xiaoqi
في
Allografts
,
Antisense RNA
,
Biological properties
2017
Hepatocellular carcinoma (HCC) is one of the most common malignant tumours with a poor prognosis worldwide. While early stage tumours can be treated with curative approaches such as liver transplantation or surgical resection, these are only suitable for a minority of patients. Those with advanced stage disease are only suitable for supportive approaches and most are resistant to the conventional chemotherapy or radiotherapy. Liver cancer stem cells (LCSCs) are a small subset of cancer cells with unlimited differentiation ability and tumour forming potential. In order to develop novel therapeutic approaches for HCC, we need to understand how the cancer develops and why treatment resistance occurs. Using high-throughput sequencing techniques, a large number of dysregulated long noncoding RNAs (lncRNAs) have been identified, and some of which are closely linked to key aspects of liver cancer pathology, progression, outcomes and for the maintenance of cancer stem cell-like properties. In addition, some lncRNAs are potential biomarkers for HCC diagnosis and may serve as the therapeutic targets. This review summarizes data recently reported lncRNAs that might be critical for the maintenance of the biological properties of LCSCs.
Journal Article
Gastric cancer-derived exosomal miR-519a-3p promotes liver metastasis by inducing intrahepatic M2-like macrophage-mediated angiogenesis
2022
Background Liver metastasis (LM) is a major obstacle to the prognosis of gastric cancer (GC) patients, but the molecular mechanism underlying gastric cancer liver metastasis (GC-LM) remains unknown. Exosomes have been identified as an important mediator of communication between tumor cells and the microenvironment. Therefore, we sought to investigate the effects of primary GC cells on the liver microenvironment and the role of exosomal microRNAs (exo-miRNA) in GC-LM. Methods Sequential differential centrifugation, transmission electron microscopy and NanoSight analysis were used to extract and characterize exosomes. MicroRNA sequencing in GC-derived exosomes and mRNA sequencing in PMA-treated THP-1 cells were used to identify differentially expressed miRNAs in exosomes and the functional targets of exosomal miR-519a-3p (exo-miR-519a-3p) in macrophages, respectively. Tracing and internalization of exosomes and transfer of exo-miR-519a-3p were observed by immunofluorescence. Tubule formation assays, aortic ring assays, and exosome-educated GC-LM model were used to investigate the roles of GC-derived exosomes and exo-miR-519a-3p in angiogenesis and GC-LM. Luciferase reporter assay, qRT-PCR, Western blot, ELISA, flow cytometry and immunofluorescence were used to investigate the regulatory mechanism of exo-miR-519a-3p at GC-LM. Results The expression level of miR-519a-3p in serum exosomes was significantly higher in GC-LM patients than in patients without LM, and high expression of exo-miR-519a-3p indicates a worse prognosis. GC-derived exosomes are mainly accumulated in the liver and internalized by intrahepatic macrophages. Mechanistically, exo-miR-519a-3p activates the MAPK/ERK pathway by targeting DUSP2, thereby causing M2-like polarization of macrophages. M2-like polarized macrophages accelerate GC-LM by inducing angiogenesis and promoting intrahepatic premetastatic niche formation. Conclusions Our results indicate that exo-miR-519a-3p plays a critical role in mediating crosstalk between primary GC cells and intrahepatic macrophages and is a potential therapeutic target for GC-LM. Keywords: Gastric cancer liver metastasis, Exosomes, miR-519a-3p, M2-like polarization, Angiogenesis
Journal Article
The Immunoscore system predicts prognosis after liver metastasectomy in colorectal cancer liver metastases
2018
Background
The Immunoscore was initially established to evaluate the prognosis of stage I/II/III colorectal cancer patients. However, the feasibility of the Immunoscore for the prognosis of colorectal cancer liver metastases (CRCLM) has not been reported.
Methods
Liver metastases in 249 CRCLM patients were retrospectively analyzed. The Immunoscore was assessed according to the counts and densities of CD3+ and CD8+ T cells in the central- and peritumoral areas by immunohistochemistry. The prognostic role of the Immunoscore for relapse–free survival (RFS) and overall survival (OS) was analyzed with Kaplan–Meier curves and Cox multivariate models, and confirmed via an internal validation. Receiver operating characteristic (ROC) curves were plotted to compare the prognostic values of the Immunoscore and the clinical risk score (CRS) system.
Results
CRCLM patients with high Immunoscores (> 2) had significantly longer RFS [median RFS (95% confidence interval; 95% CI) 21.4 (7.8–35.1) vs. 8.7 (6.8–10.5) months,
P
< 0.001] and OS [median OS (95% CI): not reached vs. 28.7 (23.2–34.2) months,
P
< 0.001] than those with low Immunoscores (≤ 2). After stratification by CRS, the Immunoscore retained a statistically significant prognostic value for OS. The areas under the ROC curves (AUROCs) of the Immunoscore and the CRS system for RFS were 0.711 [95% CI 0.642–0.781] and 0.675[95% CI 0.601–0.749] (
P
= 0.492), whereas the AUROC of the Immunoscore system for OS was larger than that of the CRS system [0.759 (95% CI 0.699–0.818) vs. 0.660 (95% CI 0.592–0.727);
P
= 0.029].
Conclusions
The Immunoscore of liver metastases can be applied to predict the prognosis of CRCLM patients following liver resection.
Journal Article
KLK10 derived from tumor endothelial cells accelerates colon cancer cell proliferation and hematogenous liver metastasis formation
بواسطة
Noda, Takehiro
,
Kobayashi, Shogo
,
Shimizu, Junzo
في
Angiogenesis inhibitors
,
Animals
,
Antibodies
2024
Tumor endothelial cells (TECs), which are thought to be structurally and functionally different from normal endothelial cells (NECs), are increasingly attracting attention as a therapeutic target in hypervascular malignancies. Although colorectal liver metastasis (CRLM) tumors are hypovascular, inhibitors of angiogenesis are a key drug in multidisciplinary therapy, and TECs might be involved in the development and progression of cancer. Here, we analyzed the function of TEC in the CRLM tumor microenvironment. We used a murine colon cancer cell line (CT26) and isolated TECs from CRLM tumors. TECs showed higher proliferation and migration than NECs. Coinjection of CT26 and TECs yielded rapid tumor formation in vivo. Immunofluorescence analysis showed that coinjection of CT26 and TECs increased vessel formation and Ki-67
cells. Transcriptome analysis identified kallikrein-related peptide 10 (KLK10) as a candidate target. Coinjection of CT26 and TECs after KLK10 downregulation with siRNA suppressed tumor formation in vivo. TEC secretion of KLK10 decreased after KLK10 downregulation, and conditioned medium after KLK10 knockdown in TECs suppressed CT26 proliferative activity. Double immunofluorescence staining of KLK10 and CD31 in CRLM tissues revealed a significant correlation between poor prognosis and positive KLK10 expression in TECs and tumor cells. On multivariate analysis, KLK10 expression was an independent prognostic factor in disease-free survival. In conclusion, KLK10 derived from TECs accelerates colon cancer cell proliferation and hematogenous liver metastasis formation. KLK10 in TECs might offer a promising therapeutic target in CRLM.
Journal Article
Phase II trial on SBRT for unresectable liver metastases: long-term outcome and prognostic factors of survival after 5 years of follow-up
بواسطة
Tomatis, Stefano
,
Iftode, Cristina
,
Reggiori, Giacomo
في
Aged
,
Cancer metastasis
,
Cancer therapies
2018
The aim of this study was to evaluate long-term efficacy and survival prognostic factors of stereotactic body radiation therapy (SBRT) for un-resectable liver metastases in patients enrolled in a prospective phase II trial.
5-year local control (LC), overall survival (OS), progression free survival (PFS) and toxicity rates were analyzed in patients with un-resectable liver metastases enrolled in a Phase II Trial on liver SBRT, with a prescription dose of 75Gy in 3 consecutive fractions.
A total of 61 patients with 76 lesions were enrolled, with a median follow-up time of 6.1 years. One, three and 5 year LC rates were 94 ± 3.1%, 78.0 ± 5.9% and 78.0 ± 5.9%, without reaching the median LC time. Median OS was 27.6 months and the survival rates were 85.2 ± 4.5%, 31.1 ± 5.9% and 18.0 ± 4.9% at 1, 3 and 5-year after SBRT, respectively. Univariate analysis showed that favorable primary site (colorectal, breast and gynecological) of metastases (p = 0.001) improved survival. Toxicity was moderate. One patient experienced G3 late chest wall pain, which resolved within 1 year from SBRT. No cases of Radiation Induced Liver Disease (RILD) were detected.
Long-term results of this Phase II study suggest the efficacy and safety of SBRT for un-resectable liver metastases after 5-year of follow up. Selection of cases with positive prognostic factors may improve long-term survival of these oligo-metastastic patients and may confirm the role of SBRT as an effective alternative local therapy for liver metastases.
Journal Article