Catalogue Search | MBRL
Search Results Heading
Explore the vast range of titles available.
MBRLSearchResults
-
DisciplineDiscipline
-
Is Peer ReviewedIs Peer Reviewed
-
Reading LevelReading Level
-
Content TypeContent Type
-
YearFrom:-To:
-
More FiltersMore FiltersItem TypeIs Full-Text AvailableSubjectCountry Of PublicationPublisherSourceTarget AudienceDonorLanguagePlace of PublicationContributorsLocation
Done
Filters
Reset
514
result(s) for
"Cooper, Jamie"
Sort by:
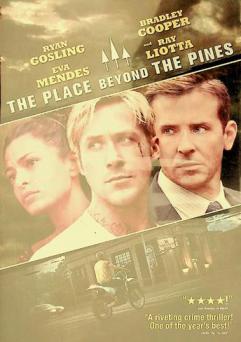
The place beyond the Pines
by
Cianfrance, Derek screenwriter, film director
,
Coccio, Ben, 1975- screenwriter
,
Marder, Darius screenwriter
in
Thieves Drama
,
Crime Drama
2012
A motorcycle stunt rider turns to robbing banks as a way to provide for his lover and their newborn child, a decision that puts him on a collision course with an ambitious rookie cop navigating a department ruled by a corrupt detective.
Systemic Inflammatory Response Syndrome Criteria in Defining Severe Sepsis
by
Kaukonen, Kirsi-Maija
,
Cooper, D. Jamie
,
Bellomo, Rinaldo
in
Aged
,
Australia
,
Databases, Factual
2015
Sepsis remains a major global cause of morbidity and death. This investigation from Australia and New Zealand ICUs challenges the utility of the two criteria of the systemic inflammatory response syndrome as a key element in defining severe sepsis.
Severe sepsis is a major cause of admission to the intensive care unit (ICU) and death.
1
,
2
The criteria according to the systemic inflammatory response syndrome (SIRS) were described 23 years ago as a clinical expression of the host response to inflammation.
3
In this context and in the presence of symptoms meeting two or more SIRS criteria, severe sepsis was seen as evolving from infection to sepsis, severe sepsis, and septic shock, in order of increasing severity. This approach was codified by the consensus statement of the American College of Chest Physicians and Society of Critical Care Medicine in 1992 . . .
Journal Article
Longitudinal Weight Gain and Related Risk Behaviors during the COVID-19 Pandemic in Adults in the US
2021
Cross-sectional analyses have shown increased obesogenic behaviors and a potential for weight gain during COVID-19 related peak-lockdown (March–May 2020), but longitudinal data are lacking. This study assessed longitudinal changes in body weight and lifestyle behaviors in the US adults during the pandemic. Methods: We used Qualtrics survey to collect self-reported data on body weight, dietary, physical activity, and psychological variables (n = 727) during the peak-lockdown (April/May) and at post-lockdown (September/October). Peak-lockdown weight data were categorized based on the magnitude of weight gained, maintained, or lost, and behavioral differences were examined between categories at two time points. Results: Body weight increased (+0.62 kg; p < 0.05) at the post-lockdown period. The body mass index also increased (26.38 ± 5.98 kg/m2 vs. 26.12 ± 5.81 kg/m2; p < 0.01) at the post-lockdown period vs. peak-lockdown period. Close to 40% of participants reported gaining either 1–4 lbs or >5 lbs of body weight during the peak-lockdown, while 18.2% lost weight. Weight-gainers engaged in riskier dietary behaviors such as frequent ultra-processed food intake (p < 0.01) and snacking (p < 0.001), were less active, and reported high stress and less craving control during peak-lockdown. Of those gaining >5 lbs, 33% continued to gain weight after the lockdown eased, while 28% maintain higher body weight. In weight-gainers, takeout meal frequency increased, and high ultra-processed food intake and stress, and low craving control continued to persist after the lockdown eased. Conclusion: We show that the COVID-19 lockdown periods disrupted weight management among many Americans and that associated health effects are likely to persist.
Journal Article
A management algorithm for adult patients with both brain oxygen and intracranial pressure monitoring: the Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC)
by
Taccone, Fabio Silvio
,
Romer, Geocadin
,
Stocchetti Nino
in
Algorithms
,
Blood transfusion
,
Brain
2020
BackgroundCurrent guidelines for the treatment of adult severe traumatic brain injury (sTBI) consist of high-quality evidence reports, but they are no longer accompanied by management protocols, as these require expert opinion to bridge the gap between published evidence and patient care. We aimed to establish a modern sTBI protocol for adult patients with both intracranial pressure (ICP) and brain oxygen monitors in place.MethodsOur consensus working group consisted of 42 experienced and actively practicing sTBI opinion leaders from six continents. Having previously established a protocol for the treatment of patients with ICP monitoring alone, we addressed patients who have a brain oxygen monitor in addition to an ICP monitor. The management protocols were developed through a Delphi-method-based consensus approach and were finalized at an in-person meeting.ResultsWe established three distinct treatment protocols, each with three tiers whereby higher tiers involve therapies with higher risk. One protocol addresses the management of ICP elevation when brain oxygenation is normal. A second addresses management of brain hypoxia with normal ICP. The third protocol addresses the situation when both intracranial hypertension and brain hypoxia are present. The panel considered issues pertaining to blood transfusion and ventilator management when designing the different algorithms.ConclusionsThese protocols are intended to assist clinicians in the management of patients with both ICP and brain oxygen monitors but they do not reflect either a standard-of-care or a substitute for thoughtful individualized management. These protocols should be used in conjunction with recommendations for basic care, management of critical neuroworsening and weaning treatment recently published in conjunction with the Seattle International Brain Injury Consensus Conference.
Journal Article
Predicting Survival after Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Failure. The Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) Score
by
Sheldrake, Jayne
,
Aubron, Cecile
,
Combes, Alain
in
Adult
,
Anesthesia. Intensive care medicine. Transfusions. Cell therapy and gene therapy
,
Australia - epidemiology
2014
Increasing use of extracorporeal membrane oxygenation (ECMO) for acute respiratory failure may increase resource requirements and hospital costs. Better prediction of survival in these patients may improve resource use, allow risk-adjusted comparison of center-specific outcomes, and help clinicians to target patients most likely to benefit from ECMO.
To create a model for predicting hospital survival at initiation of ECMO for respiratory failure.
Adult patients with severe acute respiratory failure treated by ECMO from 2000 to 2012 were extracted from the Extracorporeal Life Support Organization (ELSO) international registry. Multivariable logistic regression was used to create the Respiratory ECMO Survival Prediction (RESP) score using bootstrapping methodology with internal and external validation.
Of the 2,355 patients included in the study, 1,338 patients (57%) were discharged alive from hospital. The RESP score was developed using pre-ECMO variables independently associated with hospital survival on logistic regression, which included age, immunocompromised status, duration of mechanical ventilation before ECMO, diagnosis, central nervous system dysfunction, acute associated nonpulmonary infection, neuromuscular blockade agents or nitric oxide use, bicarbonate infusion, cardiac arrest, PaCO2, and peak inspiratory pressure. The receiver operating characteristics curve analysis of the RESP score was c = 0.74 (95% confidence interval, 0.72-0.76). External validation, performed on 140 patients, exhibited excellent discrimination (c = 0.92; 95% confidence interval, 0.89-0.97).
The RESP score is a relevant and validated tool to predict survival for patients receiving ECMO for respiratory failure.
Journal Article
Effect of dietary fatty acid composition on substrate utilization and body weight maintenance in humans
by
Krishnan, Sridevi
,
Cooper, Jamie A
in
Adaptation, Physiological
,
adverse effects
,
Biological and medical sciences
2014
BACKGROUND/PURPOSE: Dietary fat content is a primary factor associated with the increase in global obesity rates. There is a delay in achieving fat balance following exposure to a high-fat (HF) diet (≥ 40 % of total energy from fat) and fat balance is closely linked to energy balance. Exercise has been shown to improve this rate of adaptation to a HF diet. Recently, however, the role of dietary fatty acid composition on energy and macronutrient balance has come into question. METHODS: We chose studies that compared monounsaturated fatty acids (MUFA), polyunsaturated fatty acids (PUFA), and saturated fatty acids (SFA). We have reviewed studies that measured diet-induced thermogenesis (DIT), energy expenditure (EE), or fat oxidation (FOx) in response to a HF meal challenge, or long-term dietary intervention comparing these fatty acids. RESULTS: While single-meal studies show that SFA induce lower DIT and FOx compared to unsaturated fats, the effect of the degree of unsaturation (MUFA vs. PUFA) appears to yet be determined. Long-term dietary interventions also support the notion that unsaturated fats induce greater EE, DIT, and/or FOx versus SFA and that a high MUFA diet induces more weight loss compared to a high SFA diet. Sex and BMI status also affect the metabolic responses to different fatty acids; however, more research in these areas is warranted. CONCLUSION: SFA are likely more obesigenic than MUFA, and PUFA. The unsaturated fats appear to be more metabolically beneficial, specifically MUFA ≥ PUFA > SFA, as evidenced by the higher DIT and FOx following HF meals or diets.
Journal Article
Factors affecting circulating levels of peptide YY in humans: a comprehensive review
2014
As obesity continues to be a global epidemic, research into the mechanisms of hunger and satiety and how those signals act to regulate energy homeostasis persists. Peptide YY (PYY) is an acute satiety signal released upon nutrient ingestion and has been shown to decrease food intake when administered exogenously. More recently, investigators have studied how different factors influence PYY release and circulating levels in humans. Some of these factors include exercise, macronutrient composition of the diet, body-weight status, adiposity levels, sex, race and ageing. The present article provides a succinct and comprehensive review of the recent literature published on the different factors that influence PYY release and circulating levels in humans. Where human data are insufficient, evidence in animal or cell models is summarised. Additionally, the present review explores the recent findings on PYY responses to different dietary fatty acids and how this new line of research will make an impact on future studies on PYY. Human demographics, such as sex and age, do not appear to influence PYY levels. Conversely, adiposity or BMI, race and acute exercise all influence circulating PYY levels. Both dietary fat and protein strongly stimulate PYY release. Furthermore, MUFA appear to result in a smaller PYY response compared with SFA and PUFA. PYY levels appear to be affected by acute exercise, macronutrient composition, adiposity, race and the composition of fatty acids from dietary fat.
Journal Article
Predictors of return to work in survivors of critical illness
by
Hodgson, Carol L.
,
Higgins, Alisa M.
,
Myles, Paul S.
in
Brain research
,
Cognition & reasoning
,
Cognitive ability
2018
To determine predictors of inability to return to work due to health six-months after intensive care admission; and compare functional recovery between patients who had not returned to work and employed patients.
Participants were working adults admitted to ICU who received >24 h of mechanical ventilation. Outcomes included inability to return to work due to health at six-months post-ICU admission, disability, health status, anxiety, depression and post-traumatic stress.
Of 107 patients, 31 (29%) were unable to return to work due to health at six-months after ICU admission. Predictors of inability to return to work included longer hospital stay (odds ratio [OR], 1.05; 95% confidence interval [CI], 1.02–1.08; P = .004); lower Glasgow Coma Scale (GCS) at admission (OR, 0.86; CI, 0.75–0.99; P = .03); and admission due to major trauma (OR, 8.83; CI, 2.57–30.38; P < .001). Compared to employed patients, those who had not returned to work reported higher levels of disability and psychological distress, and poorer health-related quality of life.
Major trauma, lower GCS and increased hospital length of stay predicted inability to return to work due to health at six-months post-ICU admission. Compared to employed patients, those who had not returned to work reported poorer functional recovery.
•One third of patients mechanically ventilated for >24 h had not returned to work at six months due to their health.•Predictors of being unable to return to work due to poor health included increased hospital length of stay, major trauma and lower Glasgow Coma Scale.•Inability to return to work due to health was associated with anxiety, depression, post-traumatic stress and reduced health related quality of life.
Journal Article
Reduction of adverse effects from intravenous acetylcysteine treatment for paracetamol poisoning: a randomised controlled trial
by
Coyle, Judy
,
Veiraiah, Aravindan
,
Thomas, Simon H L
in
Acetaminophen - antagonists & inhibitors
,
Acetaminophen - poisoning
,
Acetylcysteine
2014
Paracetamol poisoning is common worldwide. It is treated with intravenous acetylcysteine, but the standard regimen is complex and associated with frequent adverse effects related to concentration, which can cause treatment interruption. We aimed to ascertain whether adverse effects could be reduced with either a shorter modified acetylcysteine schedule, antiemetic pretreatment, or both.
We undertook a double-blind, randomised factorial study at three UK hospitals, between Sept 6, 2010, and Dec 31, 2012. We randomly allocated patients with acute paracetamol overdose to either the standard intravenous acetylcysteine regimen (duration 20·25 h) or a shorter (12 h) modified protocol, with or without intravenous ondansetron pretreatment (4 mg). Masking was achieved by infusion of 5% dextrose (during acetylcysteine delivery) or saline (for antiemetic pretreatment). Randomisation was done via the internet and included a minimisation procedure by prognostic factors. The primary outcome was absence of vomiting, retching, or need for rescue antiemetic treatment at 2 h. Prespecified secondary outcomes included a greater than 50% increase in alanine aminotransferase activity over the admission value. Analysis was by intention to treat. This trial is registered with ClinicalTrials.gov (identifier NCT01050270).
Of 222 patients who underwent randomisation, 217 were assessable 2 h after the start of acetylcysteine treatment. Vomiting, retching, or need for rescue antiemetic treatment at 2 h was reported in 39 of 108 patients assigned to the shorter modified protocol compared with 71 of 109 allocated to the standard acetylcysteine regimen (adjusted odds ratio 0·26, 97·5% CI 0·13–0·52; p<0·0001), and in 45 of 109 patients who received ondansetron compared with 65 of 108 allocated placebo (0·41, 0·20–0·80; p=0·003). Severe anaphylactoid reactions were recorded in five patients assigned to the shorter modified acetylcysteine regimen versus 31 who were allocated to the standard protocol (adjusted common odds ratio 0·23, 97·5% CI 0·12–0·43; p<0·0001). The proportion of patients with a 50% increase in alanine aminotransferase activity did not differ between the standard (13/101) and shorter modified (9/100) regimens (adjusted odds ratio 0·60, 97·5% CI 0·20–1·83); however, the proportion was higher with ondansetron (16/100) than with placebo (6/101; 3·30, 1·01–10·72; p=0·024).
In patients with paracetamol poisoning, a 12 h modified acetylcysteine regimen resulted in less vomiting, fewer anaphylactoid reactions, and reduced need for treatment interruption. This study was not powered to detect non-inferiority of the shorter protocol versus the standard approach; therefore, further research is needed to confirm the efficacy of the 12 h modified acetylcysteine regimen.
Chief Scientist Office of the Scottish Government.
Journal Article