Catalogue Search | MBRL
Search Results Heading
Explore the vast range of titles available.
MBRLSearchResults
-
DisciplineDiscipline
-
Is Peer ReviewedIs Peer Reviewed
-
Reading LevelReading Level
-
Content TypeContent Type
-
YearFrom:-To:
-
More FiltersMore FiltersItem TypeIs Full-Text AvailableSubjectCountry Of PublicationPublisherSourceTarget AudienceDonorLanguagePlace of PublicationContributorsLocation
Done
Filters
Reset
790
result(s) for
"Howard, Helen"
Sort by:
Teacher evaluation in second language education
\"Effective language learning depends on effective instruction. In order to investigate whether or not this is taking place, teachers' classroom pedagogical practices, both in-service and pre-service, are frequently monitored by means of observation and feedback. However, research indicates that although this process has potential value for teacher learning and development, there are also a number of attendant problems and it is therefore important that practitioners share their experience with others in the field in order to expand the existing knowledge base. This volume investigates participant experiences, looking beyond the materials used and examining the way in which language teachers are evaluated and supported throughout their careers. Particular attention is given to the practices and frameworks involved, outlining key approaches and discussing tools for investigation and collaboration. The book highlights the importance of the use of talk to foster reflection and teacher learning, the value of learning from experienced others and the importance of giving voice to all those involved in the process of development and evaluation\"-- Provided by publisher.
The DANTE trial protocol: a randomised phase III trial to evaluate the Duration of ANti-PD-1 monoclonal antibody Treatment in patients with metastatic mElanoma
by
Bestall, Janine
,
Howard, Helen
,
Katona, Eszter
in
Anti-PD-1
,
Antibodies, Monoclonal - pharmacology
,
Antibodies, Monoclonal - therapeutic use
2021
Background
Immunotherapy is revolutionising the treatment of patients diagnosed with melanoma and other cancers. The first immune checkpoint inhibitor, ipilimumab (targeting cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4)), showed a survival advantage over standard chemotherapy. Subsequently the anti-programmed cell death protein 1 (PD-1) antibodies, nivolumab and pembrolizumab were shown to be more effective than ipilimumab. Ipilimumab combined with nivolumab gives an incremental gain in overall survival compared with nivolumab alone but increases the risk of severe, potentially life-threatening toxicities. In contrast to ipilimumab monotherapy, anti-PD-1 antibodies are licensed to be continued until disease progression. Follow-up of patients recruited to the first trials evaluating 2 years of pembrolizumab showed that three-quarters of responding patients continue responding after stopping treatment. Suggestive of early response, we hypothesised that continuing anti-PD-1 treatment beyond 1 year in progression-free patients may be unnecessary and so designed the DANTE trial.
Methods
DANTE is a multicentre, randomised, phase III, non-inferiority trial to evaluate the duration of anti-PD-1 therapy in patients with metastatic (unresectable stage III and stage IV) melanoma. It uses a two-stage recruitment strategy, registering patients before they complete 1 year of first-line anti-PD-1 +/− CTLA-4 therapy and randomising eligible patients who have received 12 months of treatment and are progression-free at 1 year. At randomisation, 1208 patients are assigned (1:1) to either 1) continue anti-PD-1 treatment until disease progression/ unacceptable toxicity/ for at least 2 years in the absence of disease progression/ unacceptable toxicity or 2) to stop treatment. Randomisation stratifies for baseline prognostic factors. The primary outcome is progression-free survival at 3, 6, 9 and 12 months and then, 6-monthly for up to 4-years. Secondary outcomes collected at all timepoints include overall survival, response-rate and duration and safety, with quality of life and cost-effectiveness outcomes collected 3-monthly for up to 18-months. Sub-studies include a qualitative analysis of patient acceptance of randomisation and sample collection to inform future translational studies into response/ toxicity biomarkers.
Discussion
DANTE is a unique prospective trial investigating the optimal duration of anti-PD-1 therapy in metastatic melanoma patients. Outcomes will inform future use of these high burden drugs.
Trial registration
ISRCTN15837212
, 31 July 2018.
Journal Article
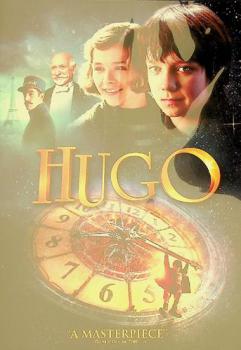
Hugo
by
Scorsese, Martin film director, film producer
,
Logan, John, 1961- writer
,
King, Graham, 1961- film producer
in
Méliès, Georges, 1861-1938 Drama
,
Robots Drama
,
Paris (France) History 1870-1940 Drama
2000
Orphan, clock keeper, and thief, twelve-year-old Hugo lives in the walls of a busy Paris train station, where his survival depends on secrets and anonymity. But when his world suddenly interlocks with an eccentric girl and the owner of a small toy booth in the train station, Hugo's undercover life, and his most precious secret, are put in jeopardy. A cryptic drawing, a treasured notebook, a stolen key, a mechanical man, and a hidden message all come together to change Hugo's life forever.
PRISM protocol: a randomised phase II trial of nivolumab in combination with alternatively scheduled ipilimumab in first-line treatment of patients with advanced or metastatic renal cell carcinoma
2019
Background
The combination of nivolumab, a programmed death-1 (PD-1) targeted monoclonal antibody, with the cytotoxic T-lymphocyte antigen-4 (CTLA-4) targeted antibody, ipilimumab, represents a new standard of care in the first-line setting for patients with intermediate- and poor-risk metastatic renal cell carcinoma (mRCC) based on recent phase III data. Combining ipilimumab with nivolumab increases rates of grade 3 and 4 toxicity compared with nivolumab alone, and the optimal scheduling of these agents when used together remains unknown. The aim of the PRISM study is to assess whether less frequent dosing of ipilimumab (12-weekly versus 3-weekly), in combination with nivolumab, is associated with a favourable toxicity profile without adversely impacting efficacy.
Methods
The PRISM trial is a UK-based, open label, multi-centre, phase II, randomised controlled trial. The trial population consists of patients with untreated locally advanced or metastatic clear cell RCC, and aims to recruit 189 participants. Participants will be randomised on a 2:1 basis in favour of a modified schedule of 4 doses of 12-weekly ipilimumab versus a standard schedule of 4 doses of 3-weekly ipilimumab, both in combination with standard nivolumab. The proportion of participants experiencing a grade 3 or 4 adverse reaction within 12 months forms the primary endpoint of the study, but with 12-month progression free survival a key secondary endpoint. The incidence of all adverse events, discontinuation rates, overall response rate, duration of response, overall survival rates and health related quality of life will also be analysed as secondary endpoints. In addition, the potential of circulating and tissue-based biomarkers as predictors of therapy response will be explored.
Discussion
The combination of nivolumab with ipilimumab is active in patients with mRCC. Modifying the frequency of ipilimumab dosing may mitigate toxicity rates and positively impact quality of life without compromising efficacy, a hypothesis being explored in other tumour types such as non-small cell lung cancer. The best way to give this combination to patients with mRCC must be similarly established.
Trial registration
PRISM is registered with ISRCTN (reference
ISRCTN95351638
, 19/12/2017).
Trial status
At the time of submission, PRISM is open to recruitment and data collection is ongoing.
Journal Article
The Unexpected Discovery of Syngenite on Margarito d’Arezzo’s The Virgin and Child Enthroned, with Scenes of the Nativity and the Lives of the Saints (Probably 1263–4) and Its Possible Use as a Yellow Lake Substrate
by
Najorka, Jens
,
Kirby, Jo
,
Howard, Helen
in
Chromatography
,
Identification
,
organic colourants
2023
The oldest painting in the National Gallery collection, The Virgin and Child Enthroned by Margarito d’Arezzo (NG564), dated to about 1263–4, depicts the Virgin and Child in a mandorla, surrounded by scenes of the Nativity and lives of the saints, set within red and decorative black borders, against a gilded background. The materials and technique were investigated using a combination of non-invasive techniques, such as Fibre Optic Reflectance Spectroscopy (FORS) and macro X-ray fluorescence scanning (MA-XRF), and the analysis of a small number of paint samples using energy dispersive X-ray analysis in the scanning electron microscope (SEM-EDS), High-Performance Liquid Chromatography (HPLC), Attenuated Total Reflectance—Fourier transform infrared spectroscopy (ATR-FTIR) and micro X-ray Diffraction (micro-XRD). The results provided evidence for the use of a number of organic colourants, with both indigo and red lake pigments identified. The finding of an unusual compound, syngenite (K2Ca(SO4)2·H2O), is here postulated as a potential substrate for an organic yellow lake pigment. In addition, reference pigments were prepared to explore this hypothesis. Although documentary evidence confirms that yellow lakes were being produced from an early date, there is very little direct evidence for their use in 13th-century panel paintings.
Journal Article
Pharmacokinetics and pharmacodynamics of a single dose Nilotinib in individuals with Parkinson's disease
by
Moussa, Charbel
,
Hebron, Michaeline L.
,
Yusuf, Nadia
in
3,4-Dihydroxyphenylacetic Acid - cerebrospinal fluid
,
3,4-Dihydroxyphenylacetic Acid - metabolism
,
Adult
2019
Nilotinib is a broad‐based tyrosine kinase inhibitor with the highest affinity to inhibit Abelson (c‐Abl) and discoidin domain receptors (DDR1/2). Preclinical evidence indicates that Nilotinib reduces the level of brain alpha‐synuclein and attenuates inflammation in models of Parkinson's disease (PD). We previously showed that Nilotinib penetrates the blood‐brain barrier (BBB) and potentially improves clinical outcomes in individuals with PD and dementia with Lewy bodies (DLB). We performed a physiologically based population pharmacokinetic/pharmacodynamic (popPK/PD) study to determine the effects of Nilotinib in a cohort of 75 PD participants. Participants were randomized (1:1:1:1:1) into five groups (n = 15) and received open‐label random single dose (RSD) 150:200:300:400 mg Nilotinib vs placebo. Plasma and cerebrospinal fluid (CSF) were collected at 1, 2, 3, and 4 hours after Nilotinib administration. The results show that Nilotinib enters the brain in a dose‐independent manner and 200 mg Nilotinib increases the level of 3,4‐Dihydroxyphenylacetic acid (DOPAC) and homovanillic acid (HVA), suggesting alteration to dopamine metabolism. Nilotinib significantly reduces plasma total alpha‐synuclein and appears to reduce CSF oligomeric: total alpha‐synuclein ratio. Furthermore, Nilotinib significantly increases the CSF level of triggering receptors on myeloid cells (TREM)‐2, suggesting an anti‐inflammatory effect. Taken together, 200 mg Nilotinib appears to be an optimal single dose that concurrently reduces inflammation and engages surrogate disease biomarkers, including dopamine metabolism and alpha‐synuclein.
Journal Article
First UK patient cohort treated with stereotactic ablative radiotherapy for primary kidney cancer
2023
Aims Stereotactic ablative radiotherapy (SABR) for primary renal cell carcinoma (RCC) is a promising non‐invasive ablative treatment option. A prospective interventional clinical trial published showed that treatment was feasible and well tolerated. We present the first single‐institution UK cohort of patients with primary RCC receiving protocol‐based SABR with prospective follow‐up. We also present a protocol that could be used to facilitate more widespread use of the treatment. Materials and methods Nineteen biopsy‐proven primary RCC patients were treated with either 42 Gy in three fractions on alternate days or 26 Gy in a single fraction based on predefined eligibility criteria using either Linear Accelerator or CyberKnife platform. Prospective toxicity data using CTCAE V4.0 and outcome data such as estimated glomerular filtration rate (eGFR) and tumour response using CT thorax, abdomen and pelvis (CT‐TAP) were collected at 6 weeks, 3, 6, 12, 18 and 24 months post treatment. Results The 19 patients had a median age of 76 years (interquartile range [IQR] 64–82 years) and 47.4% were males, and they had a median tumour size of 4.5 cm (IQR 3.8–5.2 cm). Single and fractionated treatment was well tolerated and there were no significant acute side effects. The mean drop from baseline in eGFR at 6 months was 5.4 ml/min and that at 12 months was 8.7 ml/min. The overall local control rate at both 6 and 12 months was 94.4%. Overall survival at 6 and 12 months was 94.7% and 78.3%, respectively. After a median follow‐up of 17 months, three patients experienced a Grade 3 toxicity, which was resolved with conservative management. Conclusion SABR for primary RCC is a safe and feasible treatment for medically unfit patients, which can be delivered in most UK cancer centres using standard Linear Accelerator as well as CyberKnife platforms.
Journal Article
Addition of gemcitabine to paclitaxel, epirubicin, and cyclophosphamide adjuvant chemotherapy for women with early-stage breast cancer (tAnGo): final 10-year follow-up of an open-label, randomised, phase 3 trial
by
Howard, Helen C
,
Rea, Daniel W
,
Dodwell, David
in
Anthracycline
,
Antineoplastic Combined Chemotherapy Protocols - adverse effects
,
Antineoplastic Combined Chemotherapy Protocols - therapeutic use
2017
The tAnGo trial was designed to investigate the potential role of gemcitabine when added to anthracycline and taxane-containing adjuvant chemotherapy for early breast cancer. When this study was developed, gemcitabine had shown significant activity in metastatic breast cancer, and there was evidence of a favourable interaction with paclitaxel.
tAnGo was an international, open-label, randomised, phase 3 superiority trial that enrolled women aged 18 years or older with newly diagnosed, early-stage breast cancer who had a definite indication for chemotherapy, any nodal status, any hormone receptor status, Eastern Cooperative Oncology Group performance status of 0–1, and adequate bone marrow, hepatic, and renal function. Women were recruited from 127 clinical centres and hospitals in the UK and Ireland, and randomly assigned (1:1) to one of two treatment regimens: epirubicin, cyclophosphamide, and paclitaxel (four cycles of 90 mg/m2 intravenously administered epirubicin and 600 mg/m2 intravenously administered cyclophosphamide on day 1 every 3 weeks, followed by four cycles of 175 mg/m2 paclitaxel as a 3 h infusion on day 1 every 3 weeks) or epirubicin, cyclophosphamide, and paclitaxel plus gemcitabine (the same chemotherapy regimen as the other group, with the addition of 1250 mg/m2 gemcitabine to the paclitaxel cycles, administered intravenously as a 0·5 h infusion on days 1 and 8 every 3 weeks). Patients were randomly assigned by a central computerised deterministic minimisation procedure, with stratification by country, age, radiotherapy intent, nodal status, and oestrogen receptor and HER-2 status. The primary endpoint was disease-free survival and the trial aimed to detect 5% differences in 5-year disease-free survival between the treatment groups. Recruitment completed in 2004 and this is the final, intention-to-treat analysis. This trial is registered with EudraCT (2004-002927-41), ISRCTN (51146252), and ClinicalTrials.gov (NCT00039546).
Between Aug 22, 2001, and Nov 26, 2004, 3152 patients were enrolled and randomly assigned to epirubicin, cyclophosphamide, paclitaxel, and gemcitabine (gemcitabine group; n=1576) or to epirubicin, cyclophosphamide, and paclitaxel (control group; n=1576). 11 patients (six in the gemcitabine group and five in the control group) were ineligible because of pre-existing metastases and were therefore excluded from the analysis. At this protocol-specified final analysis (median follow-up 10 years [IQR 10–10]), 1087 disease-free survival events and 914 deaths had occurred. Disease-free survival did not differ significantly between the treatment groups at 10 years (65% [63–68] in the gemcitabine group vs 65% [62–67] in the control group), and median disease-free survival was not reached (adjusted hazard ratio 0·97 [95% CI 0·86–1·10], p=0·64). Toxicity, dose intensity, and a detailed safety substudy showed both regimens to be safe, deliverable, and tolerable. Grade 3 and 4 toxicities were reported at expected levels in both groups. The most common were neutropenia (527 [34%] of 1565 patients in the gemcitabine group vs 412 [26%] of 1567 in the control group), myalgia and arthralgia (207 [13%] vs 186 [12%]), fatigue (207 [13%] vs 152 [10%]), infection (202 [13%] vs 141 [9%]), vomiting (143 [9%] vs 108 [7%]), and nausea (132 [8%] vs 102 [7%]).
The addition of gemcitabine to anthracycline and taxane-based adjuvant chemotherapy at this dose and schedule confers no therapeutic advantage in terms of disease-free survival in early breast cancer, although it can cause increased toxicity. Therefore, gemcitabine has not been added to standard adjuvant chemotherapy in breast cancer for any subgroup.
Cancer Research UK core funding for Clinical Trials Unit at the University of Birmingham, Eli Lilly, Bristol-Myers Squibb, and Pfizer.
Journal Article
The STAR trial protocol: a randomised multi-stage phase II/III study of Sunitinib comparing temporary cessation with allowing continuation, at the time of maximal radiological response, in the first-line treatment of locally advanced/metastatic Renal Cancer
by
Howard, Helen
,
Selby, Peter J
,
Brown, Janet
in
Adult
,
Aged
,
Antineoplastic Agents - economics
2012
Background
Over recent years a number of novel therapies have shown promise in advanced renal cell carcinoma (RCC). Internationally the standard of care of first-line therapy is sunitinib™, after a clear survival benefit was demonstrated over interferon-α. Convention dictates that sunitinib is continued until evidence of disease progression, assuming tolerability, although there is no evidence that this approach is superior to intermittent periods of treatment. The purpose of the STAR trial is to compare the standard treatment strategy (conventional continuation strategy, CCS) with a novel drug free interval strategy (DFIS) which includes planned treatment breaks.
Methods/Design
The STAR trial is an NIHR HTA-funded UK pragmatic randomised phase II/III clinical trial in the first-line treatment of advanced RCC. Participants will be randomised (1:1) to either a sunitinib CCS or a DFIS. The overall aim of the trial is to determine whether a DFIS is non-inferior, in terms of 2-year overall survival (OS) and quality adjusted life years (QALY) (averaged over treatment and follow up), compared to a CCS. The QALY primary endpoint was selected to assess whether any detriment in terms of OS could be balanced with improvements in quality of life (QoL). This is a complex trial with a number of design challenges, and to address these issues a feasibility stage is incorporated into the trial design. Predetermined recruitment (stage A) and efficacy (stage B) intermediary endpoints must be met to allow continuation to the overall phase III trial (stage C). An integral qualitative patient preference and understanding study will occur alongside the feasibility stage to investigate patients’ feelings regarding participation or non-participation in the trial.
Discussion
The optimal duration of continuing sunitinib in advanced RCC is unknown. Novel targeted therapies do not always have the same constraints to treatment duration as standard chemotherapeutic agents and currently there are no randomised data comparing different treatment durations. Incorporating planned treatment breaks has the potential to improve QoL and cost effectiveness, hopefully without significant detriment on OS, as has been demonstrated in other cancer types with other treatments.
Trial Registration
Controlled-trials.com ISRCTN 06473203
Journal Article
4564 Nilotinib alters microRNAs that regulate specific autophagy and ubiquitination genes in the cerebrospinal fluid of Parkinson’s patients
by
Chiu, Timothy
,
Hebron, Michaeline
,
Willmarth, Barbara
in
Autophagy
,
Bayesian analysis
,
Cerebrospinal fluid
2020
OBJECTIVES/GOALS: Our preclinical data demonstrate that the principal effects of nilotinib, a multi-tyrosine kinase inhibitor, in models of neurodegeneration is clearance of misfolded proteins via autophagy. Here we aimed to evaluate the effects of nilotinib on microRNAs in the cerebrospinal fluid of Parkinson’s disease patients. METHODS/STUDY POPULATION: Cerebrospinal fluid (CSF) was collected as part of an open label phase I (NCT02281474) (n = 12, 300 mg nilotinib taken orally once daily for 6 months), and a phase II randomized, double-blind, placebo-controlled study (NCT02954978) (n = 75, randomized 1:1:1 into placebo, 150 mg or 300 mg nilotinib taken orally once daily for 12 months). RNA was isolated from CSF and Indexed sequencing libraries were prepared from total RNA plus miRNA. Next generation whole-genome sequencing (single-end 1x75 bp, 25 million raw reads per sample) was performed to identify miRNAs significantly differentially expressed (fold-change ≥ 2, Benjamini-Hochberg FDR p-value ≤ 0.05 or Empirical Bayes FDR ≤ 0.05) with treatment compared to baseline. RESULTS/ANTICIPATED RESULTS: Next generation whole-genome sequencing of microRNAs in the CSF demonstrated that nilotinib significantly increases microRNAs that specifically regulate expression of autophagy and ubiquitination genes in individuals with Parkinson’s disease. In the open label phase I, samples, 28 microRNAs found to regulate autophagy and ubiquitination genes, were significantly altered with treatment (Benjamini-Hochberg FDR p-value ≤ 0.05). In the phase II randomized, double-blind, placebo-controlled study samples, we verified several of those 28 candidate microRNAs had been significantly deferentially expressed with treatment (Empirical Bayes FDR p-value ≤ 0.05). DISCUSSION/SIGNIFICANCE OF IMPACT: Our data provide robust evidence that nilotinib’s effects on misfolded protein clearance is via autophagy and CSF miRNA sequencing is a valid biomarker of nilotinib’s effects in a definitive phase III study to investigate nilotinib in Parkinson’s and other neurodegenerative diseases. CONFLICT OF INTEREST DESCRIPTION: Charbel Moussa is listed as an inventor on several Georgetown University patents for the use of tyrosine kinase inhibitors as a treatment for neurodegenerative diseases
Journal Article