Catalogue Search | MBRL
Search Results Heading
Explore the vast range of titles available.
MBRLSearchResults
-
DisciplineDiscipline
-
Is Peer ReviewedIs Peer Reviewed
-
Series TitleSeries Title
-
Reading LevelReading Level
-
YearFrom:-To:
-
More FiltersMore FiltersContent TypeItem TypeIs Full-Text AvailableSubjectCountry Of PublicationPublisherSourceTarget AudienceLanguagePlace of PublicationContributorsLocation
Done
Filters
Reset
115
result(s) for
"Job, Jennifer"
Sort by:
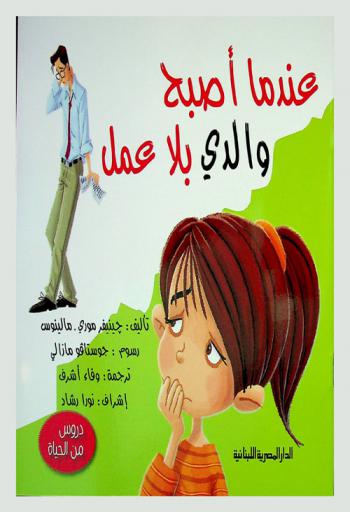
عندما أصبح والدي بلا عمل
by
Moore-Mallinos, Jennifer مؤلف
,
Mazali, Gustavo رسام
,
أشرف، وفاء مترجم
in
القصص الإنجليزية للأطفال قرن 21
,
أدب الأطفال قرن 21
2018
(دروس من الحياة) هذه السلسلة تعتمد على تقديم دروس وقيم حياتية ترتبط بشدة بحياة الأطفال وأسرهم في مختلف المواقف، مقدمة الحلول الرائعة لهذه الظروف الحياتية من خلال أسلوب حواري سلسو لكي يتعملوا منها، مدعوما برسوم بسيطة تناسب الأطفال وما يتسمون به من رغبة في مواجهة أي مواقف جديدة في حياتهم.
Implementing a general practitioner-to-general physician eConsult service (eConsultant) in Australia
by
Calleja, Zoe
,
Nicholson, Caroline
,
Donald, Maria
in
Digital infrastructure
,
eConsult
,
Electronic consultation: general practice
2022
Background
In response to lengthy wait times for specialist outpatient appointments, electronic consultation (eConsult) services have developed globally, providing asynchronous, secure and timely communication between general practitioner (GP) and specialist. This study aims to track adoption of a Queensland eConsultant service in two Australian Primary Health Networks (Western Queensland and Brisbane South) to understand key barriers and enablers to adoption and inform modification of the implementation strategy.
Methods
Our theory-informed mixed-methods evaluation assessed implementation between July 2020 and March 2022. Adoption and implementation activities were prospectively recorded in bespoke tracking spreadsheets with implementation activities coded against the Expert Recommendations for Implementing Change (ERIC) strategies. Semi-structured interviews with GPs and stakeholders informed by the Consolidated Framework for Implementation Research (CFIR) were conducted to understand determinants of implementation.
Results
Of the 40 practices invited to take part in the eConsultant service, 20 (50%) enrolled. Of the 97 GPs who consented, 38 sent at least one Request for Advice (RFA) to the eConsultant with a total of 112 RFA sent. Implementation was predominantly guided by eight strategies. Qualitative interviews were conducted with 11 GPs and 4 stakeholders (12 from rural/remote regions, 11 females and two sole practitioners). Interviewees felt the eConsultant service supported outpatient appointment avoidance and provided efficient, timely access to specialist support for GPs and their patients. Barriers identified to using eConsultant related to digital infrastructure, competing priorities, and keeping the service ‘front of mind’. Key enablers identified were the relative advantage of eConsultant over other options, patient benefits and COVD-19 facilitating the use of digital technology.
Conclusions
This evaluation highlighted service enablers as well as user priorities for broader implementation. A focus on a well-integrated digital system and availability of a variety of eConsultant specialties are seen as key strategies to embedding the eConsultant option in GP advice processes in Australia.
Journal Article
Evaluation of the Healthy Living after Cancer text message-delivered, extended contact intervention using the RE-AIM framework
by
Eakin, Elizabeth G.
,
Job, Jennifer R.
,
Fjeldsoe, Brianna S.
in
Behavior
,
Biomedical and Life Sciences
,
Biomedicine
2021
Background
Text message-delivered interventions have potential to prevent weight regain and maintain diet and physical activity behaviours through extending contact with participants following initial weight loss, lifestyle interventions. Using the RE-AIM Framework, this study evaluated the adoption, reach, implementation, effectiveness, and maintenance of an extended contact text-message intervention following the Healthy Living after Cancer (HLaC) program. HLaC was a 6-month, telephone-delivered intervention targeting healthy diet, physical activity and weight loss for adult cancer survivors, offered by Cancer Councils (CCs) in Australia.
Methods
HLaC completers (
n
= 182) were offered extended contact via text messages for 6-months (HLaC+Txt). Text message content/frequency was individually tailored to participant’s preferences, ascertained through two telephone-tailoring interviews with CC staff. Adoption (HLaC+Txt uptake among eligible CCs), reach (uptake by HLaC completers) and implementation (intervention cost/length; text dose) were assessed. The effectiveness of extended contact relative to historic controls was quantified by pre-to-post HLaC+Txt changes in self-reported: weight, moderate-vigorous physical activity (MVPA), fruit and vegetable intake, fat and fibre behaviour. Maintenance, following 6-months of noncontact for the intervention cohort, was assessed for these same variables. Semi-structured interviews with CC staff and participants contextualised outcomes.
Results
HLaC+Txt was adopted by all four CCs who had delivered HLaC. In total, 115 participants commenced HLaC+Txt, with reach ranging across CCs from 47 to 80% of eligible participants. The mean number of weeks participants received the text message intervention ranged across CCs from 18.5–22.2 weeks. Participants received (median, 25th,75th percentile) 83 (48, 119) texts, ranging across CCs from 40 to 112. The total cost of HLaC+Txt delivery was on average $AUD85.00/participant. No meaningful (
p
< 0.05) differences in self-reported outcomes were seen between HLaC+Txt and control cohorts. After 6-months no contact the intervention cohort had maintained weight, fruit intake, fat and fibre index scores relative to end of HLaC+Txt outcomes. Participants/CC staff perceived an important intervention component was maintaining accountability.
Conclusions
While feasible to implement, HLaC+Txt was not effective in the short term. However, intervention effects during the non-contact period suggest the program supports longer term maintenance of weight and diet behaviour. Intervention delivery in this real-world context highlighted key considerations for future implementation.
Trial registration
Australian and New Zealand Clinical Trials Registry (ANZCTR) -
ACTRN12615000882527
(registered on 24/08/2015).
Journal Article
The Queensland Virtual Integrated Practice (VIP) partnership program pilot study: an Australian-first model of care to support rural general practice
by
Kerrigan, Natalie
,
Lepre, Breanna
,
Martin, Zena
in
Chronic diseases
,
Continuity of care
,
Data collection
2023
Background
There is a critical lack of medical workforce internationally, and this is particularly notable in rural and remote Australia where strategies to address workforce shortages are urgently required. This pilot study aimed to implement and evaluate a Virtual Integrated Practice (VIP) Program in the Australian rural primary care setting.
Methods
The VIP model was developed using co-creation methodology and involves an urban GP joining a rural general practice team to provide ongoing care to patients remotely via secure telehealth. The pilot study was conducted in two western Queensland general practices, commencing in October 2021 with one rural practice and extending to an additional rural practice from November 2022. Evaluation included a retrospective review of service, billing and cost data, and an online survey for patients. Ethical approval was obtained from the University of Queensland Human Research Ethics Committee (Project number: 2021/HE002434).
Results
There were 1468 services provided through to December 2022, including general consults (n = 1197), therapeutic procedures (n = 68), mental health treatment plans (n = 68) and chronic disease management plans (n = 59). Patients were predominantly female (73.1%) and did not have their appointment at the practice (57.8%). Among 1282 occasions of service, less than 20% of consultations (n = 224) required support from staff (e.g., a nurse), and more than half were repeat patient encounters (53.0%). Survey respondents (n = 45) indicated that they were satisfied (9.3%) or highly satisfied (90.7%) with the care provided, and importantly, 95.5% of respondents reported that the service improved their access to the GP. More than 20% of respondents indicated that they would attend the Emergency Department if virtual care was not available.
Conclusions
Data from this pilot study has informed translation to an additional 20 vulnerable rural general practices in three further rural regions in Queensland in 2023 and evaluation is ongoing. This pilot study demonstrates the feasibility and acceptability of an innovative, digitally supported community-focussed, healthcare initiative to arrest the decline in rural general practice workforce, improve patient care access and support rural practice viability.
Journal Article
Dose and engagement during an extended contact physical activity and dietary behavior change intervention delivered via tailored text messaging: exploring relationships with behavioral outcomes
by
Goode, Ana D
,
Spilsbury, Kate L
,
Eakin, Elizabeth G
in
accelerometry
,
Behavior
,
behavior change
2021
Background
Extended contact interventions delivered via text messaging are a low-cost option for promoting the long-term continuation of behavior change. This secondary analysis of a text message–delivered extended contact intervention (‘Get Healthy, Stay Healthy’ (GHSH)) explores the extent to which changes in physical activity, dietary behaviors and body weight were associated with the frequency of text messages (dose) and contact between the health coach and participant (engagement).
Methods
Following a telephone coaching program, participants were randomised to receive extended contact via tailored text messages (GHSH,
n
= 114) or no additional contact (
n
= 114) over a 6-month period. Message dose, timing, and content were based on participant preferences, ascertained during two tailoring telephone calls. All incoming and outgoing messages were recorded. At baseline and 6 months, participants self-reported body weight and dietary behaviors (fruit and vegetable servings/day). Moderate-vigorous physical activity (MVPA) was assessed via accelerometry.
Results
Median dose (25th, 75th percentile) was 53 (33, 72) text messages in total across six months. Mean fortnightly dose in weeks 1–2 was 5.5 (95 % CI: 4.3, 6.6) text messages, and remained stable (with the exception of planned decreases in weeks involving additional intervention contacts). Offset against the average fortnightly dose of goal checks (1.6, 95 % CI: 1.3, 2.0 and 1.5, 95 % CI: 1.2, 1.8, for physical activity and diet respectively), mean replies to goal checks were highest in weeks 1–2 (1.4, 95 % CI: 1.4, 1.5 and 1.3, 95 % CI: 1.2, 1.4, respectively) and tended to become lower in most weeks thereafter. Greater weight loss was positively associated with text message dose (
P
= 0.022), with a difference of 1.9 kg between participants receiving the most and fewest texts. There was no association between engagement and changes in outcome measures.
Conclusions
A fixed dose of texts does not seem suitable to meet participants’ individual preferences. Higher self-selected text doses predicted better weight outcomes. However, greater participant engagement through text replies does not predict more favourable outcomes, despite being a suggested facilitator of successful behavior change maintenance.
Trial registration
Australian New Zealand Clinical Trials Registry number: ACTRN12613000949785. Date registered: 27 August 2013. Retrospectively registered.
http://www.anzctr.org.au/
.
Journal Article
Mobile Health Biometrics to Enhance Exercise and Physical Activity Adherence in Type 2 Diabetes (MOTIVATE-T2D): a decentralised feasibility randomised controlled trial delivered across the UK and Canada
2025
ObjectivesAssess the feasibility of a mobile health (mHealth)-supported home-delivered physical activity (PA) intervention (MOTIVATE-T2D) in people with recently diagnosed type 2 diabetes (T2D).DesignFeasibility multicentre, parallel group, randomised controlled trial (RCT).SettingParticipants were recruited from England and Canada using a decentralised design.ParticipantsAdults (40–75 years) recently diagnosed with T2D (5–24 months).InterventionsParticipants were randomised 1:1 to intervention (MOTIVATE-T2D) or active control groups. Participants codesigned 6month- home-delivered, personalised, progressive PA programmes supported by virtual behavioural counselling. MOTIVATE-T2D used biofeedback from wearable technologies to support the programme. The active control group received the same intervention without wearables.OutcomesThe primary outcomes were recruitment rate, retention and adherence to purposeful exercise. Clinical data on effectiveness were collected as exploratory outcomes at baseline, 6 and 12 months, with HbA1c and systolic blood pressure (BP) proposed as primary outcomes for a future full RCT.Resultsn=135 eligible participants expressed an interest in the trial, resulting in 125 participants randomised (age 55±9 years, 48% female, 81% white), a recruitment rate of 93%. Retention at 12 months was 82%. MOTIVATE-T2D participants were more likely to start (OR 10.4, CI 3.4 to 32.1) and maintain purposeful exercise at 6 (OR 7.1, CI 3.2 to 15.7) and 12 months (OR 2.9, CI 1.2 to 7.4). Exploratory clinical outcomes showed a potential effect in favour of MOTIVATE-T2D, including proposed primary outcomes HbA1c and systolic BP (between-group mean differences: HbA1c: 6 months: −5% change from baseline, CI −10 to 2: 12 months: −2% change from baseline, CI −8 to −4; systolic BP: 6 months: −1 mm Hg, CI −5 to 3: 12 months: −4 mm Hg, CI −8 to 1).ConclusionsOur findings support the feasibility of delivering the MOTIVATE-T2D mHealth-supported PA intervention for people with recently diagnosed T2D and progression to a full RCT to examine its clinical and cost-effectiveness.Trial registration numberISRCTN: 14335124; ClinicalTrials.gov: NCT0465353.
Journal Article
Translating research into practice: outcomes from the Healthy Living after Cancer partnership project
by
Hiller, Janet E.
,
Winkler, Elisabeth A. H.
,
Boyle, Frances
in
Alliances and partnerships
,
Analysis
,
Behavior
2020
Background
Healthy Living after Cancer (HLaC) was a national dissemination and implementation study of an evidence-based lifestyle intervention for cancer survivors. The program was imbedded into existing telephone cancer information and support services delivered by Australian state-based Cancer Councils (CC). We report here the reach, effectiveness, adoption, implementation, and maintenance of the program.
Methods
In this phase IV study (single-group, pre-post design) participants - survivors of any type of cancer, following treatment with curative intent - received up to 12 nurse/allied health professional-led telephone health coaching calls over 6 months. Intervention delivery was grounded in motivational interviewing, with emphasis on evidence-based behaviour change strategies. Using the RE-AIM evaluation framework, primary outcomes were reach, indicators of program adoption, implementation, costs and maintenance. Secondary (effectiveness) outcomes were participant-reported anthropometric, behavioural and psychosocial variables including: weight; physical activity; dietary intake; quality-of-life; treatment side-effects; distress; and fear of cancer recurrence and participant satisfaction. Changes were evaluated using linear mixed models, including terms for timepoint (0/6 months), strata (Cancer Council), and timepoint x strata.
Results
Four of 5 CCs approached participated in the study. In total, 1183 cancer survivors were referred (mostly via calls to the Cancer Council telephone information service). Of these, 90.4% were eligible and 88.7% (
n
= 791) of those eligible consented to participate. Retention rate was 63.4%. Participants were mostly female (88%), aged 57 years and were overweight (BMI = 28.8 ± 6.5 kg/m2). Improvements in all participant-reported outcomes (standardised effect sizes of 0.1 to 0.6) were observed (
p
< 0.001). The program delivery costs were on average AU$427 (US$296) per referred cancer survivor.
Conclusions
This telephone-delivered lifestyle intervention, which was feasibly implemented by Cancer Councils, led to meaningful and statistically significant improvements in cancer survivors’ health and quality-of-life at a relatively low cost.
Trial registration
Australian and New Zealand Clinical Trials Registry (ANZCTR) -
ACTRN12615000882527
(registered on 24/08/2015).
Journal Article
Feasibility of an asynchronous general practitioner-to-general physician eConsultant outpatient substitution program: A Queensland pilot study
by
Caroline Nicholson
,
Jennifer Job
,
Jan Chaffey
in
Health facilities
,
Hospitals
,
Outpatient services
2021
Background and objective: The use of an 'eConsultant' to support the family physician is an established outpatient substitution model in North America. This pilot study investigates the feasibility of the eConsultant model for complex chronic disease management within the Australian setting.
Methods: This pilot study was implemented in one urban and four rural/remote general practices in one state. The general practitioner (GP) sent a request for advice (RFA), a clinical summary with a specific clinical question/s, via secure messaging to a physician working remotely. Responses were required for GP/patient follow-up within 72 hours.
Results: The mean (standard deviation [SD]) time for general physician reply was 2.1 (1.2) days, and mean (SD) time from initial to subsequent GP/patient review was 14.8 (16.7) days. Only 13.3% of eConsultations required a subsequent face-to-face outpatient department appointment.
Discussion: The eConsultant model is feasible in Australia, with potential for improving access and reducing time to non-GP specialist input.
Journal Article
Living well after breast cancer randomized controlled trial protocol: evaluating a telephone-delivered weight loss intervention versus usual care in women following treatment for breast cancer
2016
Background
Obesity, physical inactivity and poor diet quality have been associated with increased risk of breast cancer-specific and all-cause mortality as well as treatment-related side-effects in breast cancer survivors. Weight loss intervention trials in breast cancer survivors have shown that weight loss is safe and achievable; however, few studies have examined the benefits of such interventions on a broad range of outcomes and few have examined factors important to translation (e.g. feasible delivery method for scaling up, assessment of sustained changes, cost-effectiveness). The Living Well after Breast Cancer randomized controlled trial aims to evaluate a 12-month telephone-delivered weight loss intervention (versus usual care) on weight change and a range of secondary outcomes including cost-effectiveness.
Methods/design
Women (18–75 years; body mass index 25–45 kg/m
2
) diagnosed with stage I-III breast cancer in the previous 2 years are recruited from public and private hospitals and through the state-based cancer registry (target
n
= 156). Following baseline assessment, participants are randomized 1:1 to either a 12-month telephone-delivered weight loss intervention (targeting diet and physical activity) or usual care. Data are collected at baseline, 6-months (mid-intervention), 12-months (end-of-intervention) and 18-months (maintenance). The primary outcome is change in weight at 12-months. Secondary outcomes are changes in body composition, bone mineral density, cardio-metabolic and cancer-related biomarkers, metabolic health and chronic disease risk, physical function, patient-reported outcomes (quality of life, fatigue, menopausal symptoms, body image, fear of cancer recurrence) and behaviors (dietary intake, physical activity, sitting time). Data collected at 18-months will be used to assess whether outcomes achieved at end-of-intervention are sustained six months after intervention completion. Cost-effectiveness will be assessed, as will mediators and moderators of intervention effects.
Discussion
This trial will provide evidence needed to inform the wide-scale provision of weight loss, physical activity and dietary interventions as part of routine survivorship care for breast cancer survivors.
Trial registration
Australian and New Zealand Clinical Trial Registry (ANZCTR) -
ACTRN12612000997853
(Registered 18 September 2012).
Journal Article
Women’s Perceptions of Participation in an Extended Contact Text Message–Based Weight Loss Intervention: An Explorative Study
2017
Extending contact with participants after the end of an initial weight loss intervention has been shown to lead to maintained weight loss and related behavioral change. Mobile phone text messaging (short message service, SMS) offers a low-cost and efficacious method to deliver extended contact. In this rapidly developing area, formative work is required to understand user perspectives of text message technology. An extended contact intervention delivered by text messages following an initial telephone-delivered weight loss intervention in breast cancer survivors provided this opportunity.
The aim of this study was to qualitatively explore women's perceptions of participation in an extended contact intervention using text messaging to support long-term weight loss, physical activity, and dietary behavioral change.
Following the end of an initial 6-month randomized controlled trial of a telephone-delivered weight loss intervention (versus usual care), participants received a 6-month extended contact intervention via tailored text messages. Participant perceptions of the different types of text messages, the content, tailoring, timing, and frequency of the text messages, and the length of the intervention were assessed through semistructured interviews conducted after the extended contact intervention. The interviews were transcribed verbatim and analyzed with key themes identified.
Participants (n=27) were a mean age of 56.0 years (SD 7.8) and mean body mass index of 30.4 kg/m2 (SD 4.2) and were at a mean of 16.1 months (SD 3.1) postdiagnosis at study baseline. Participants perceived the text messages to be useful behavioral prompts and felt the messages kept them accountable to their behavioral change goals. The individual tailoring of the text message content and schedules was a key to the acceptability of the messages; however, some women preferred the support and real-time discussion via telephone calls (during the initial intervention) compared with the text messages (during the extended contact intervention).
Text message support was perceived as acceptable for the majority of women as a way of extending intervention contact for weight loss and behavioral maintenance. Text messages supported the maintenance of healthy behaviors established in the intervention phase and kept the women accountable to their goals. A combination of telephone calls and text message support was suggested as a more acceptable option for some of the women for an extended contact intervention.
Journal Article