Catalogue Search | MBRL
Search Results Heading
Explore the vast range of titles available.
MBRLSearchResults
-
DisciplineDiscipline
-
Is Peer ReviewedIs Peer Reviewed
-
Series TitleSeries Title
-
Reading LevelReading Level
-
YearFrom:-To:
-
More FiltersMore FiltersContent TypeItem TypeIs Full-Text AvailableSubjectCountry Of PublicationPublisherSourceTarget AudienceLanguagePlace of PublicationContributorsLocation
Done
Filters
Reset
1,377
result(s) for
"Via, E."
Sort by:
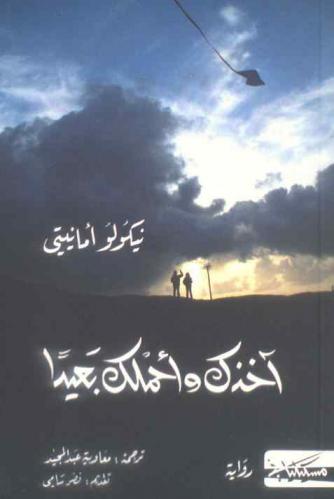
آخذك وأحملك بعيدا
by
Ammaniti, Niccolò, 1966- مؤلف
,
عبد الحميد، معاوية مترجم
,
سامي، نصر مقدم
in
القصص الإيطالية قرن 21
2016
رواية (آخذك وأحملك بعيدا) للكاتب الإيطالي (نيكولو أمانيتي) ترجمة (معاوية عبد المجيد) هي رواية درامية بالدرجة الأولى، تتداخل فيها حيوات الشخصيات لتشكل مزيجا متكاملا، فهي رواية رومانسية عالية التشويق تتناول معاني مختلفة لفهم الحياة، وترصد حياة شخصيات مختلفة فيما بينها أشد الاختلاف يجمعها فقط بلدة صغيرة تدعى \"ايسكيانو\"، وتتميز الرواية بالعمق والزخم.. فهي تحكي عن الشخصيات وتقدمها بعمق، كما أنها تتميز بكثرة عدد الشخصيات، بالنسبة للبطل الذي يقول الراوي إنه البطل الرئيسي في الرواية وهو \"بييترو\" هو طفل مسكين، يتعرض لمضايقات من عصابة \"فيديريكو\" ولا يدافع عن نفسه وإنما يستسلم تماما، يتكور على نفسه حين يهمون بضربه ويتلقى الضربات الموجعة ويرحل، وحين أجبروه على مصاحبتهم في إحدى الأعمال الشريرة رضخ دون مقاومة، فقد أجبروه على وضع قفل على باب المدرسة حتى يهربوا من تسليم واجباتهم المدرسية، وحين كشفهم الحارس وقاومهم تعرض \"بييترو\" لرصاصة طائشة ثم وشى به الحارس، واضطر هو أن يعترف على العصابة ووعدته المعلمة \"فلورا\" أنه لن يرسب هذا العام، لكنها لم تساعده لأنها بدورها تعرضت لأزمة في حياتها نتيجة لاستكانتها وضعفها. فالكاتب يريد أن يقول على لسان أبطاله، أن الضعيف يخسر دوما، حيث إن الناس يستهينون به ويؤذونه، وقد قالت له المعلمة \"فلورا\" ذلك حين تسلل \"بييترو\" إلى منزلها، لكي يعاقبها على نكثها لوعدها له، لكنه وجدها في حالة مزرية وقد أصابتها نوبة جنون وحين صارحته بضعفه وأن الناس يستهينون به لأنه لا يقوى على رد الشر عنه دفعها بيديه فتأذت رأسها من حوض الاستحمام وماتت... إلخ.
Tuberculosis drugs’ distribution and emergence of resistance in patient’s lung lesions: A mechanistic model and tool for regimen and dose optimization
2019
The sites of mycobacterial infection in the lungs of tuberculosis (TB) patients have complex structures and poor vascularization, which obstructs drug distribution to these hard-to-reach and hard-to-treat disease sites, further leading to suboptimal drug concentrations, resulting in compromised TB treatment response and resistance development. Quantifying lesion-specific drug uptake and pharmacokinetics (PKs) in TB patients is necessary to optimize treatment regimens at all infection sites, to identify patients at risk, to improve existing regimens, and to advance development of novel regimens. Using drug-level data in plasma and from 9 distinct pulmonary lesion types (vascular, avascular, and mixed) obtained from 15 hard-to-treat TB patients who failed TB treatments and therefore underwent lung resection surgery, we quantified the distribution and the penetration of 7 major TB drugs at these sites, and we provide novel tools for treatment optimization.
A total of 329 plasma- and 1,362 tissue-specific drug concentrations from 9 distinct lung lesion types were obtained according to optimal PK sampling schema from 15 patients (10 men, 5 women, aged 23 to 58) undergoing lung resection surgery (clinical study NCT00816426 performed in South Korea between 9 June 2010 and 24 June 2014). Seven major TB drugs (rifampin [RIF], isoniazid [INH], linezolid [LZD], moxifloxacin [MFX], clofazimine [CFZ], pyrazinamide [PZA], and kanamycin [KAN]) were quantified. We developed and evaluated a site-of-action mechanistic PK model using nonlinear mixed effects methodology. We quantified population- and patient-specific lesion/plasma ratios (RPLs), dynamics, and variability of drug uptake into each lesion for each drug. CFZ and MFX had higher drug exposures in lesions compared to plasma (median RPL 2.37, range across lesions 1.26-22.03); RIF, PZA, and LZD showed moderate yet suboptimal lesion penetration (median RPL 0.61, range 0.21-2.4), while INH and KAN showed poor tissue penetration (median RPL 0.4, range 0.03-0.73). Stochastic PK/pharmacodynamic (PD) simulations were carried out to evaluate current regimen combinations and dosing guidelines in distinct patient strata. Patients receiving standard doses of RIF and INH, who are of the lower range of exposure distribution, spent substantial periods (>12 h/d) below effective concentrations in hard-to-treat lesions, such as caseous lesions and cavities. Standard doses of INH (300 mg) and KAN (1,000 mg) did not reach therapeutic thresholds in most lesions for a majority of the population. Drugs and doses that did reach target exposure in most subjects include 400 mg MFX and 100 mg CFZ. Patients with cavitary lesions, irrespective of drug choice, have an increased likelihood of subtherapeutic concentrations, leading to a higher risk of resistance acquisition while on treatment. A limitation of this study was the small sample size of 15 patients, performed in a unique study population of TB patients who failed treatment and underwent lung resection surgery. These results still need further exploration and validation in larger and more diverse cohorts.
Our results suggest that the ability to reach and maintain therapeutic concentrations is both lesion and drug specific, indicating that stratifying patients based on disease extent, lesion types, and individual drug-susceptibility profiles may eventually be useful for guiding the selection of patient-tailored drug regimens and may lead to improved TB treatment outcomes. We provide a web-based tool to further explore this model and results at http://saviclab.org/tb-lesion/.
Journal Article
Host-directed therapy of tuberculosis based on interleukin-1 and type I interferon crosstalk
2014
Active tuberculosis has been linked to excessive type I interferon induction whereas interleukin-1 may have protective effects; here it is shown that interleukin-1 enhances the production of prostaglandin E2, which helps contain the pathogen while also suppressing detrimental type I interferon.
TB treatment targets innate immunity
Tuberculosis is re-emerging as a major threat to public health following the spread of multi-drug-resistant
Mycobacterium tuberculosis
and complications caused by the HIV epidemic. And there is still no globally effective vaccine. Now a collaboration between laboratories across the United States and in Brazil, China and India has developed an immunotherapeutic approach that targets innate immunity in a mouse tuberculosis model through the manipulation of the cytokines interferon (present in excess in active tuberculosis) and interleukin-1 (thought to have protective effects). Katrin Mayer-Barber and colleagues show that these cytokines are functionally linked through the eicosanoids. This work serves as a proof of concept for treatments directed at the host eicosanoid network, and suggests feasible alternatives to conventional chemotherapy.
Tuberculosis remains second only to HIV/AIDS as the leading cause of mortality worldwide due to a single infectious agent
1
. Despite chemotherapy, the global tuberculosis epidemic has intensified because of HIV co-infection, the lack of an effective vaccine and the emergence of multi-drug-resistant bacteria
2
,
3
,
4
,
5
. Alternative host-directed strategies could be exploited to improve treatment efficacy and outcome, contain drug-resistant strains and reduce disease severity and mortality
6
. The innate inflammatory response elicited by
Mycobacterium tuberculosis
(Mtb) represents a logical host target
7
. Here we demonstrate that interleukin-1 (IL-1) confers host resistance through the induction of eicosanoids that limit excessive type I interferon (IFN) production and foster bacterial containment. We further show that, in infected mice and patients, reduced IL-1 responses and/or excessive type I IFN induction are linked to an eicosanoid imbalance associated with disease exacerbation. Host-directed immunotherapy with clinically approved drugs that augment prostaglandin E2 levels in these settings prevented acute mortality of Mtb-infected mice. Thus, IL-1 and type I IFNs represent two major counter-regulatory classes of inflammatory cytokines that control the outcome of Mtb infection and are functionally linked via eicosanoids. Our findings establish proof of concept for host-directed treatment strategies that manipulate the host eicosanoid network and represent feasible alternatives to conventional chemotherapy.
Journal Article
High Persister Mutants in Mycobacterium tuberculosis
by
Lee, Jong Seok
,
Via, Laura E.
,
Keren, Iris
in
Animals
,
Anti-Bacterial Agents - pharmacology
,
Antibiotics
2016
Mycobacterium tuberculosis forms drug-tolerant persister cells that are the probable cause of its recalcitrance to antibiotic therapy. While genetically identical to the rest of the population, persisters are dormant, which protects them from killing by bactericidal antibiotics. The mechanism of persister formation in M. tuberculosis is not well understood. In this study, we selected for high persister (hip) mutants and characterized them by whole genome sequencing and transcriptome analysis. In parallel, we identified and characterized clinical isolates that naturally produce high levels of persisters. We compared the hip mutants obtained in vitro with clinical isolates to identify candidate persister genes. Genes involved in lipid biosynthesis, carbon metabolism, toxin-antitoxin systems, and transcriptional regulators were among those identified. We also found that clinical hip isolates exhibited greater ex vivo survival than the low persister isolates. Our data suggest that M. tuberculosis persister formation involves multiple pathways, and hip mutants may contribute to the recalcitrance of the infection.
Journal Article
Evaluation of a Rapid Molecular Drug-Susceptibility Test for Tuberculosis
2017
Increasing drug resistance in
Mycobacterium tuberculosis
complicates the management of tuberculosis. Development of a point-of-care test to determine drug susceptibility could greatly enhance care. In this report, a rapid
M. tuberculosis
diagnostic is assessed.
Journal Article
Anti-vascular endothelial growth factor treatment normalizes tuberculosis granuloma vasculature and improves small molecule delivery
2015
Tuberculosis (TB) causes almost 2 million deaths annually, and an increasing number of patients are resistant to existing therapies. Patients who have TB require lengthy chemotherapy, possibly because of poor penetration of antibiotics into granulomas where the bacilli reside. Granulomas are morphologically similar to solid cancerous tumors in that they contain hypoxic microenvironments and can be highly fibrotic. Here, we show that TB-infected rabbits have impaired small molecule distribution into these disease sites due to a functionally abnormal vasculature, with a low-molecular-weight tracer accumulating only in peripheral regions of granulomatous lesions. Granuloma-associated vessels are morphologically and spatially heterogeneous, with poor vessel pericyte coverage in both human and experimental rabbit TB granulomas. Moreover, we found enhanced VEGF expression in both species. In tumors, antiangiogenic, specifically anti-VEGF, treatments can “normalize” their vasculature, reducing hypoxia and creating a window of opportunity for concurrent chemotherapy; thus, we investigated vessel normalization in rabbit TB granulomas. Treatment of TB-infected rabbits with the anti-VEGF antibody bevacizumab significantly decreased the total number of vessels while normalizing those vessels that remained. As a result, hypoxic fractions of these granulomas were reduced and small molecule tracer delivery was increased. These findings demonstrate that bevacizumab treatment promotes vascular normalization, improves small molecule delivery, and decreases hypoxia in TB granulomas, thereby providing a potential avenue to improve delivery and efficacy of current treatment regimens.
Significance Tuberculosis (TB) is the second most lethal pathogen worldwide. Pulmonary granulomas are a hallmark of this disease. By discovering similarities between granulomas and solid cancerous tumors, we identified a novel therapeutic target for TB, the abnormal granuloma-associated vasculature that contributes to the abnormal granuloma microenvironment. We then asked if we could “normalize” granuloma vasculature by blocking VEGF signaling, an approach originally shown to enhance cancer treatment. Our results demonstrate that bevacizumab, a widely prescribed anti-VEGF antibody for cancer and eye diseases, is able to create more structurally and functionally normal granuloma vasculature and improve the delivery of a low-molecular-weight tracer. This effect suggests that vascular normalization in combination with anti-TB drugs has the potential to enhance treatment in patients with TB.
Journal Article
Plasticity of the Mycobacterium tuberculosis respiratory chain and its impact on tuberculosis drug development
2019
The viability of Mycobacterium tuberculosis (
Mtb
) depends on energy generated by its respiratory chain. Cytochrome
bc1-aa3
oxidase and type-2 NADH dehydrogenase (NDH-2) are respiratory chain components predicted to be essential, and are currently targeted for drug development. Here we demonstrate that an
Mtb
cytochrome
bc1-aa3
oxidase deletion mutant is viable and only partially attenuated in mice. Moreover, treatment of
Mtb
-infected marmosets with a cytochrome
bc1-aa3
oxidase inhibitor controls disease progression and reduces lesion-associated inflammation, but most lesions become cavitary. Deletion of both NDH-2 encoding genes (Δ
ndh-2
mutant) reveals that the essentiality of NDH-2 as shown in standard growth media is due to the presence of fatty acids. The Δ
ndh-2
mutant is only mildly attenuated in mice and not differently susceptible to clofazimine, a drug in clinical use proposed to engage NDH-2. These results demonstrate the intrinsic plasticity of
Mtb
’s respiratory chain, and highlight the challenges associated with targeting the pathogen’s respiratory enzymes for tuberculosis drug development.
New tuberculosis therapies, targeting respiratory chain components of
Mycobacterium tuberculosis
, are under development. Here the authors show that, contrary to common belief, some of these components are not essential for pathogen viability and/or virulence in animal models of infection.
Journal Article
Storage lipid studies in tuberculosis reveal that foam cell biogenesis is disease-specific
by
Bruiners, Natalie
,
Prideaux, Brendan
,
O’Brien, Paul
in
Animals
,
Atherosclerosis - metabolism
,
Atherosclerosis - pathology
2018
Foam cells are lipid-laden macrophages that contribute to the inflammation and tissue damage associated with many chronic inflammatory disorders. Although foam cell biogenesis has been extensively studied in atherosclerosis, how these cells form during a chronic infectious disease such as tuberculosis is unknown. Here we report that, unlike the cholesterol-laden cells of atherosclerosis, foam cells in tuberculous lung lesions accumulate triglycerides. Consequently, the biogenesis of foam cells varies with the underlying disease. In vitro mechanistic studies showed that triglyceride accumulation in human macrophages infected with Mycobacterium tuberculosis is mediated by TNF receptor signaling through downstream activation of the caspase cascade and the mammalian target of rapamycin complex 1 (mTORC1). These features are distinct from the known biogenesis of atherogenic foam cells and establish a new paradigm for non-atherogenic foam cell formation. Moreover, they reveal novel targets for disease-specific pharmacological interventions against maladaptive macrophage responses.
Journal Article
Linezolid for Treatment of Chronic Extensively Drug-Resistant Tuberculosis
by
Choi, Hongjo
,
Park, Hyeeun
,
Follmann, Dean
in
Acetamides - adverse effects
,
Acetamides - pharmacokinetics
,
Acetamides - therapeutic use
2012
There are limited therapeutic options for extensively drug-resistant tuberculosis. In this study from South Korea, linezolid was shown to have some activity in treating resistant tuberculosis; however, its use was associated with clinically significant toxicity.
Linezolid (Zyvox, Pfizer) was approved in 2000 for drug-resistant, gram-positive bacterial infections.
1
A member of the oxazolidinone antibiotic class, linezolid inhibits protein synthesis by binding the 23S ribosomal RNA (rRNA) portion of the bacterial 50S ribosomal subunit.
2
In adults, linezolid is administered at a dose of 600 mg twice daily, with phase 3 and postmarketing trials showing an acceptable side-effect and adverse-event profile during the FDA-approved 28 days of therapy.
3
Data on longer-term use are limited, but serious neuropathies (e.g., peripheral and optic neuropathies), myelosuppression, and hyperlactatemia have been observed
4
,
5
and are considered to be related to the inhibition . . .
Journal Article
The within-host population dynamics of Mycobacterium tuberculosis vary with treatment efficacy
2017
Background
Combination therapy is one of the most effective tools for limiting the emergence of drug resistance in pathogens. Despite the widespread adoption of combination therapy across diseases, drug resistance rates continue to rise, leading to failing treatment regimens. The mechanisms underlying treatment failure are well studied, but the processes governing successful combination therapy are poorly understood. We address this question by studying the population dynamics of
Mycobacterium tuberculosis
within tuberculosis patients undergoing treatment with different combinations of antibiotics.
Results
By combining very deep whole genome sequencing (~1000-fold genome-wide coverage) with sequential sputum sampling, we were able to detect transient genetic diversity driven by the apparently continuous turnover of minor alleles, which could serve as the source of drug-resistant bacteria. However, we report that treatment efficacy has a clear impact on the population dynamics: sufficient drug pressure bears a clear signature of purifying selection leading to apparent genetic stability. In contrast,
M. tuberculosis
populations subject to less drug pressure show markedly different dynamics, including cases of acquisition of additional drug resistance.
Conclusions
Our findings show that for a pathogen like
M. tuberculosis
, which is well adapted to the human host, purifying selection constrains the evolutionary trajectory to resistance in effectively treated individuals. Nonetheless, we also report a continuous turnover of minor variants, which could give rise to the emergence of drug resistance in cases of drug pressure weakening. Monitoring bacterial population dynamics could therefore provide an informative metric for assessing the efficacy of novel drug combinations.
Journal Article