Catalogue Search | MBRL
Search Results Heading
Explore the vast range of titles available.
MBRLSearchResults
-
DisciplineDiscipline
-
Is Peer ReviewedIs Peer Reviewed
-
Reading LevelReading Level
-
Content TypeContent Type
-
YearFrom:-To:
-
More FiltersMore FiltersItem TypeIs Full-Text AvailableSubjectCountry Of PublicationPublisherSourceTarget AudienceDonorLanguagePlace of PublicationContributorsLocation
Done
Filters
Reset
1,564
result(s) for
"Weiner, Michael"
Sort by:
Tracking pathophysiological processes in Alzheimer's disease: an updated hypothetical model of dynamic biomarkers
by
Vemuri, Prashanthi
,
Shaw, Leslie M
,
Jack, Clifford R
in
Alzheimer Disease - cerebrospinal fluid
,
Alzheimer Disease - pathology
,
Alzheimer Disease - physiopathology
2013
In 2010, we put forward a hypothetical model of the major biomarkers of Alzheimer's disease (AD). The model was received with interest because we described the temporal evolution of AD biomarkers in relation to each other and to the onset and progression of clinical symptoms. Since then, evidence has accumulated that supports the major assumptions of this model. Evidence has also appeared that challenges some of our assumptions, which has allowed us to modify our original model. Refinements to our model include indexing of individuals by time rather than clinical symptom severity; incorporation of interindividual variability in cognitive impairment associated with progression of AD pathophysiology; modifications of the specific temporal ordering of some biomarkers; and recognition that the two major proteinopathies underlying AD biomarker changes, amyloid β (Aβ) and tau, might be initiated independently in sporadic AD, in which we hypothesise that an incident Aβ pathophysiology can accelerate antecedent limbic and brainstem tauopathy.
Journal Article
Diagnostic performance and prediction of clinical progression of plasma phospho-tau181 in the Alzheimer’s Disease Neuroimaging Initiative
by
Karikari, Thomas K
,
Shaw, Leslie M
,
Saha-Chaudhuri Paramita
in
Alzheimer's disease
,
Biomarkers
,
Cerebrospinal fluid
2021
Whilst cerebrospinal fluid (CSF) and positron emission tomography (PET) biomarkers for amyloid-β (Aβ) and tau pathologies are accurate for the diagnosis of Alzheimer’s disease (AD), their broad implementation in clinical and trial settings are restricted by high cost and limited accessibility. Plasma phosphorylated-tau181 (p-tau181) is a promising blood-based biomarker that is specific for AD, correlates with cerebral Aβ and tau pathology, and predicts future cognitive decline. In this study, we report the performance of p-tau181 in >1000 individuals from the Alzheimer’s Disease Neuroimaging Initiative (ADNI), including cognitively unimpaired (CU), mild cognitive impairment (MCI) and AD dementia patients characterized by Aβ PET. We confirmed that plasma p-tau181 is increased at the preclinical stage of Alzheimer and further increases in MCI and AD dementia. Individuals clinically classified as AD dementia but having negative Aβ PET scans show little increase but plasma p-tau181 is increased if CSF Aβ has already changed prior to Aβ PET changes. Despite being a multicenter study, plasma p-tau181 demonstrated high diagnostic accuracy to identify AD dementia (AUC = 85.3%; 95% CI, 81.4–89.2%), as well as to distinguish between Aβ− and Aβ+ individuals along the Alzheimer’s continuum (AUC = 76.9%; 95% CI, 74.0–79.8%). Higher baseline concentrations of plasma p-tau181 accurately predicted future dementia and performed comparably to the baseline prediction of CSF p-tau181. Longitudinal measurements of plasma p-tau181 revealed low intra-individual variability, which could be of potential benefit in disease-modifying trials seeking a measurable response to a therapeutic target. This study adds significant weight to the growing body of evidence in the use of plasma p-tau181 as a non-invasive diagnostic and prognostic tool for AD, regardless of clinical stage, which would be of great benefit in clinical practice and a large cost-saving in clinical trial recruitment.
Journal Article
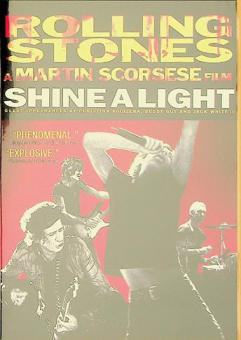
Shine a light
by
Scorsese, Martin film director
,
Cohl, Michael film producer
,
Weiner, Zane film producer
in
Rolling Stones drama
,
Rock music 2001-2010 Drama
2000
A career-spanning documentary on the Rolling Stones, with concert footage from their \"A Bigger Bang\" tour.
Cerebrospinal fluid and plasma biomarkers in Alzheimer disease
by
Hampel, Harald
,
Blennow, Kaj
,
Zetterberg, Henrik
in
692/53
,
692/699/375/365/1283
,
Alzheimer Disease
2010
The early detection of Alzheimer disease might be critical to the effectiveness of disease-modifying drugs, when such therapies become available. In this Review, Blennow
et al
. examine the use of cerebrospinal fluid and plasma biomarkers in the early diagnosis of this neurodegenerative disorder. The authors also explore roles for cerebrospinal fluid biomarkers in Alzheimer disease clinical trials.
Intense multidisciplinary research has provided detailed knowledge of the molecular pathogenesis of Alzheimer disease (AD). This knowledge has been translated into new therapeutic strategies with putative disease-modifying effects. Several of the most promising approaches, such as amyloid-β immunotherapy and secretase inhibition, are now being tested in clinical trials. Disease-modifying treatments might be at their most effective when initiated very early in the course of AD, before amyloid plaques and neurodegeneration become too widespread. Thus, biomarkers are needed that can detect AD in the predementia phase or, ideally, in presymptomatic individuals. In this Review, we present the rationales behind and the diagnostic performances of the core cerebrospinal fluid (CSF) biomarkers for AD, namely total tau, phosphorylated tau and the 42 amino acid form of amyloid-β. These biomarkers reflect AD pathology, and are candidate markers for predicting future cognitive decline in healthy individuals and the progression to dementia in patients who are cognitively impaired. We also discuss emerging plasma and CSF biomarkers, and explore new proteomics-based strategies for identifying additional CSF markers. Furthermore, we outline the roles of CSF biomarkers in drug discovery and clinical trials, and provide perspectives on AD biomarker discovery and the validation of such markers for use in the clinic.
Key Points
Current clinical diagnostic criteria for Alzheimer disease (AD) require a patient to have dementia before a diagnosis can be made, and are largely based on the exclusion of other disorders
Disease-modifying drugs for AD, when they become available, will need to be administered very early in the course of the disease, before neurodegeneration is too severe and widespread
No clinical method is available for identifying prodromal AD in patients with mild cognitive impairment (MCI), as such individuals have only mild disturbances in episodic memory
The cerebrospinal fluid (CSF) biomarkers total tau, phosphorylated tau (p-tau
181
and p-tau
231
) and β-amyloid
1–42
have a high diagnostic accuracy for AD, and for prodromal AD in patients with MCI
CSF biomarkers are increasingly being used in the clinic for diagnosing AD, and will also be valuable in clinical trials, allowing enrichment of patient populations with pure AD cases
Biomarker evidence that a candidate drug affects the central disease processes in AD will, together with a beneficial effect on cognition, be essential for labeling the drug as disease modifying
Journal Article
Living Cancer
2021
Long days, important decisions, difficult conversations. A doctor's work is never truly done. After working as a pediatric oncologist for 40 years, Dr. Michael Weiner has collected a multitude of stories. From the best case scenarios to the worst, Dr. Weiner has chosen to share some of the most memorable and heartbreaking moments of his career. Always in close contact with pain and heartbreak, his accounts express his willingness to help patients and their families through great times of need. His observations about cancer are further informed when his daughter was diagnosed with cancer as well as his own personal cancer journey.
Locally linear embedding (LLE) for MRI based Alzheimer's disease classification
2013
Modern machine learning algorithms are increasingly being used in neuroimaging studies, such as the prediction of Alzheimer's disease (AD) from structural MRI. However, finding a good representation for multivariate brain MRI features in which their essential structure is revealed and easily extractable has been difficult. We report a successful application of a machine learning framework that significantly improved the use of brain MRI for predictions. Specifically, we used the unsupervised learning algorithm of local linear embedding (LLE) to transform multivariate MRI data of regional brain volume and cortical thickness to a locally linear space with fewer dimensions, while also utilizing the global nonlinear data structure. The embedded brain features were then used to train a classifier for predicting future conversion to AD based on a baseline MRI. We tested the approach on 413 individuals from the Alzheimer's Disease Neuroimaging Initiative (ADNI) who had baseline MRI scans and complete clinical follow-ups over 3years with the following diagnoses: cognitive normal (CN; n=137), stable mild cognitive impairment (s-MCI; n=93), MCI converters to AD (c-MCI, n=97), and AD (n=86). We found that classifications using embedded MRI features generally outperformed (p<0.05) classifications using the original features directly. Moreover, the improvement from LLE was not limited to a particular classifier but worked equally well for regularized logistic regressions, support vector machines, and linear discriminant analysis. Most strikingly, using LLE significantly improved (p=0.007) predictions of MCI subjects who converted to AD and those who remained stable (accuracy/sensitivity/specificity: =0.68/0.80/0.56). In contrast, predictions using the original features performed not better than by chance (accuracy/sensitivity/specificity: =0.56/0.65/0.46). In conclusion, LLE is a very effective tool for classification studies of AD using multivariate MRI data. The improvement in predicting conversion to AD in MCI could have important implications for health management and for powering therapeutic trials by targeting non-demented subjects who later convert to AD.
•Locally linear embedding (LLE) is an unsupervised learning algorithm.•It was used to extract characteristic MR features of brain alternations.•It was used to classify normal aging subjects, MCI and AD patients from ADNI data.•The performance of predicting AD in MCIs was significantly improved by using LLE.•LLE benefitted various classifiers, such as SVM, LDA and regularized regressions.
Journal Article
Hypothetical model of dynamic biomarkers of the Alzheimer's pathological cascade
by
Petersen, Ronald C
,
Shaw, Leslie M
,
Jack, Clifford R
in
Aging - genetics
,
Aging - pathology
,
Aging - physiology
2010
Currently available evidence strongly supports the position that the initiating event in Alzheimer's disease (AD) is related to abnormal processing of β-amyloid (Aβ) peptide, ultimately leading to formation of Aβ plaques in the brain. This process occurs while individuals are still cognitively normal. Biomarkers of brain β-amyloidosis are reductions in CSF Aβ
42 and increased amyloid PET tracer retention. After a lag period, which varies from patient to patient, neuronal dysfunction and neurodegeneration become the dominant pathological processes. Biomarkers of neuronal injury and neurodegeneration are increased CSF tau and structural MRI measures of cerebral atrophy. Neurodegeneration is accompanied by synaptic dysfunction, which is indicated by decreased fluorodeoxyglucose uptake on PET. We propose a model that relates disease stage to AD biomarkers in which Aβ biomarkers become abnormal first, before neurodegenerative biomarkers and cognitive symptoms, and neurodegenerative biomarkers become abnormal later, and correlate with clinical symptom severity.
Journal Article
Acceptable performance of blood biomarker tests of amyloid pathology — recommendations from the Global CEO Initiative on Alzheimer’s Disease
by
Reilly, David
,
Mattke, Soeren
,
Somers, Elizabeth
in
Alzheimer's disease
,
Biomarkers
,
Pathology
2024
Anti-amyloid treatments for early symptomatic Alzheimer disease have recently become clinically available in some countries, which has greatly increased the need for biomarker confirmation of amyloid pathology. Blood biomarker (BBM) tests for amyloid pathology are more acceptable, accessible and scalable than amyloid PET or cerebrospinal fluid (CSF) tests, but have highly variable levels of performance. The Global CEO Initiative on Alzheimer’s Disease convened a BBM Workgroup to consider the minimum acceptable performance of BBM tests for clinical use. Amyloid PET status was identified as the reference standard. For use as a triaging test before subsequent confirmatory tests such as amyloid PET or CSF tests, the BBM Workgroup recommends that a BBM test has a sensitivity of ≥90% with a specificity of ≥85% in primary care and ≥75–85% in secondary care depending on the availability of follow-up testing. For use as a confirmatory test without follow-up tests, a BBM test should have performance equivalent to that of CSF tests — a sensitivity and specificity of ~90%. Importantly, the predictive values of all biomarker tests vary according to the pre-test probability of amyloid pathology and must be interpreted in the complete clinical context. Use of BBM tests that meet these performance standards could enable more people to receive an accurate and timely Alzheimer disease diagnosis and potentially benefit from new treatments.Anti-amyloid treatments for early symptomatic Alzheimer disease have greatly increased the need for biomarker confirmation of amyloid pathology and blood biomarker tests offer an accessible and scalable biomarker test. This Consensus Statement provides recommendations for the minimum acceptable performance of blood biomarker tests for clinical use.
Journal Article