Catalogue Search | MBRL
Search Results Heading
Explore the vast range of titles available.
MBRLSearchResults
-
DisciplineDiscipline
-
Is Peer ReviewedIs Peer Reviewed
-
Series TitleSeries Title
-
Reading LevelReading Level
-
YearFrom:-To:
-
More FiltersMore FiltersContent TypeItem TypeIs Full-Text AvailableSubjectCountry Of PublicationPublisherSourceTarget AudienceDonorLanguagePlace of PublicationContributorsLocation
Done
Filters
Reset
130,221
result(s) for
"Alcohol use"
Sort by:
Altered sleep architecture following consecutive nights of presleep alcohol
by
Gredvig-Ardito, Caroline
,
McCullar, Katie S
,
Swift, Robert M
in
Adult
,
Alcohol Drinking - adverse effects
,
Alcohol use
2024
Abstract
Study Objectives
Alcohol consumption before sleep decreases sleep latency, explaining the common use of alcohol as a sleep aid. The full impact of alcohol on sleep architecture is not well understood, particularly the potential cumulative effects of presleep alcohol consumption across consecutive nights. Here, we describe the effects of presleep alcohol on sleep architecture across three consecutive nights.
Methods
Thirty adult participants took part in a crossover, within-participants study consisting of two sets of three consecutive nights of in-lab polysomnography. For each series of nights, participants drank one of the two beverages: a mixer only or a mixer plus alcohol (targeting a BrAC of 0.08 mg/L), ending 1 hour before lights out. Polysomnography (PSG) was used to stage sleep, and standard sleep variables were extracted. Linear mixed-effect analysis and generalized additive modeling were used to examine the effect of alcohol on sleep architecture.
Results
Alcohol before sleep increased the rate of slow wave sleep (SWS) accumulation across all three nights and decreased the rate of rapid eye movement (REM) sleep accumulation at the start of each night. Alcohol also decreased the total amount of REM sleep but did not affect the total amount of SWS each night.
Conclusions
These data indicate that drinking alcohol before sleep substantially affects sleep architecture, including changes to the rate of accumulation of SWS and REM sleep. We show that alcohol disrupts normal sleep architecture, leading to a significant decrease in REM sleep; thus, the use of alcohol as a sleep aid remains a public health concern.
Graphical Abstract
Journal Article
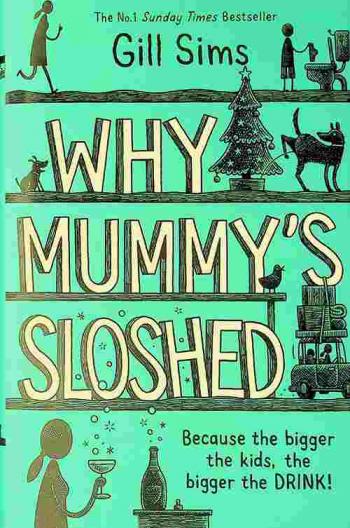
Why mummy's sloshed : because the bigger the kids, the bigger the drink!
Mummy has been a wife and mother for so long that she's a little bit lost. And despite her best efforts, her precious moppets still don't know the location of the laundry basket, the difference between being bored and being hungry, or that saying 'I can't find it Mummy' is not the same as actually looking for it. Amidst the chaos of A-Levels and driving tests, she's doing her best to keep her family afloat, even if everybody is set on drifting off in different directions, and that one of those directions is to make yet another bloody snack. She's feeling overwhelmed and underappreciated, and the only thing that Mummy knows for sure is that the bigger the kids, the bigger the drink.
Loneliness and Increased Hazardous Alcohol Use: Data from a Nationwide Internet Survey with 1-Year Follow-Up
by
Iso, Hiroyasu
,
Sugiyama, Yoshifumi
,
Kinjo, Aya
in
Alcohol Drinking - epidemiology
,
Alcohol Drinking - psychology
,
Alcohol use
2022
We aimed to examine the association between loneliness and developing alcohol dependence or hazardous alcohol use. A cohort study was conducted utilizing data from a nationwide internet survey in 2021 and 2022 in Japan. A total of 15,854 follow-up participants (55% men, with a mean age of 52.8 years) were divided based on AUDIT scores: nondrinkers (AUDIT: 0), low-risk drinkers (AUDIT: 1–7), medium-risk drinkers (AUD: 8–14), high-risk drinkers (AUDIT: 15–19), and probable alcohol dependence (AUDIT: 20–40). The University of California, Los Angeles Loneliness Scale (Version 3), a short-form three-item scale, was used to assess loneliness (high loneliness score of ≥6). The prevalence of high loneliness was higher in nondrinkers than that in low- and medium-risk drinkers, i.e., 22%, 18%, and 17%, respectively, as well as in high-risk drinkers (32%) and those with probable alcohol dependence (43%) compared to non-high-risk drinkers (19%). After adjusting for various factors (sociodemographic, social isolation, psychological distress, and smoking), non-high-risk drinkers (AUDIT: 0–14) with high loneliness were more likely to become high-or-over-risk drinkers (AUDIT: 15–40) than those without high loneliness, with adjusted risk ratios of 1.45 (95% confidence interval: 1.08–1.96) through multivariable binary logistic regression. Among non-high-risk drinkers, people with high loneliness scores at baseline were associated with increased high-risk drinking patterns with probable alcohol dependence.
Journal Article
The Use of the Alcohol Use Disorders Identification Test – Consumption as an Indicator of Hazardous Alcohol Use among University Students
by
Verhoog, Sanne
,
de Jonge, Jannet M.
,
Hoekstra, Trynke
in
Academic achievement
,
Alcohol use
,
Alcoholism
2020
Background: Hazardous drinking among students in higher education is a growing concern. The alcohol use disorders identification test (AUDIT) is the gold standard screening instrument for hazardous drinking in the adult population, for which an abbreviated version has been developed: the AUDIT-Consumption (AUDIT-C). Currently, there’s no gold standard for identifying hazardous drinking among students in higher education and little evidence regarding the concurrent validity of the AUDIT-C as a screening instrument for this group. This study investigated the concurrent validity of the AUDIT-C in a sample of university students and suggests the most appropriate cutoff points. Methods: Cross-sectional data of health surveys from 5,401 university and university of applied sciences in the Netherlands were used. Receiver operating characteristic (ROC) curves, sensitivity, specificity, and positive and negative predictive values for different cutoff scores of AUDIT-C were calculated for the total sample and for subgroups stratified by age, gender, and educational level. AUDIT-score ≥11 was used as the criterion of hazardous and harmful drinking. Results: Twenty percent of students were hazardous and harmful drinkers. The area under the ROC curve was 0.922 (95% CI 0.914–0.930). At an AUDIT-C cutoff score of ≥7, sensitivity and specificity were both >80%, while other cutoffs showed less balanced results. A cutoff of ≥8 performed better among males, but for other subgroups ≥7 was most suitable. Conclusion: AUDIT-C seems valid in identifying hazardous and harmful drinking students, with suggested optimal cutoffs 7 (females) or 8 (males). However, considerations regarding avoiding false-positives versus false-negatives, in relation to the type of intervention following screening, could lead to selecting different cutoffs.
Journal Article
Machine : a novel
\"Follows a group of teens during a seaside summer and the efforts of a guilt-driven girl to piece together the events that led to a drowning\"-- Provided by publisher.
Habits : remaking addiction
by
Moore, David
,
Keane, Helen
,
Fraser, Suzanne
in
Binge drinking
,
Compulsive behavior
,
Eating disorders
2014
What is 'addiction'? What does it say about us, our social arrangements and our political preoccupations? Where is it going as an idea and what is at stake in its ongoing production? Drawing on ethnographic research, interviews and media and policy texts, this book traces the remaking of addiction in contemporary Western societies.
National Prevalence of Alcohol and Other Substance Use Disorders Among Emergency Department Visits and Hospitalizations: NHAMCS 2014–2018
2022
BackgroundAcute healthcare utilization attributed to alcohol use disorders (AUD) and other substance use disorders (SUD) is rising.ObjectiveTo describe the prevalence and characteristics of emergency department (ED) visits and hospitalizations made by adults with AUD or SUD.Design, Setting, and ParticipantsObservational study with retrospective analysis of the National Hospital Ambulatory Medical Care Survey (2014 to 2018), a nationally representative survey of acute care visits with information on the presence of AUD or SUD abstracted from the medical chart.Main MeasuresOutcome measured as the presence of AUD or SUD.Key ResultsFrom 2014 to 2018, the annual average prevalence of AUD or SUD was 9.4% of ED visits (9.3 million visits) and 11.9% hospitalizations (1.4 million hospitalizations). Both estimates increased over time (30% and 57% relative increase for ED visits and hospitalizations, respectively, from 2014 to 2018). ED visits and hospitalizations from individuals with AUD or SUD, compared to individuals with neither AUD nor SUD, had higher percentages of Medicaid insurance (ED visits: AUD: 33.1%, SUD: 35.0%, neither: 24.4%; hospitalizations: AUD: 30.7%, SUD: 36.3%, neither: 14.8%); homelessness (ED visits: AUD: 6.2%, SUD 4.4%, neither 0.4%; hospitalizations: AUD: 5.9%, SUD 7.3%, neither: 0.4%); coexisting depression (ED visits: AUD: 26.3%, SUD 24.7%, neither 10.5%; hospitalizations: AUD: 33.5%, SUD 35.3%, neither: 13.9%); and injury/trauma (ED visits: AUD: 51.3%, SUD 36.3%, neither: 26.4%; hospitalizations: AUD: 31.8%, SUD: 23.8%, neither: 15.0%).ConclusionsIn this nationally representative study, 1 in 11 ED visits and 1 in 9 hospitalizations were made by adults with AUD or SUD, and both increased over time. These estimates are higher or similar than previous national estimates using claims data. This highlights the importance of identifying opportunities to address AUD and SUD in acute care settings in tandem with other medical concerns, particularly among visits presenting with injury, trauma, or coexisting depression.
Journal Article