Catalogue Search | MBRL
Search Results Heading
Explore the vast range of titles available.
MBRLSearchResults
-
DisciplineDiscipline
-
Is Peer ReviewedIs Peer Reviewed
-
Reading LevelReading Level
-
Content TypeContent Type
-
YearFrom:-To:
-
More FiltersMore FiltersItem TypeIs Full-Text AvailableSubjectCountry Of PublicationPublisherSourceTarget AudienceDonorLanguagePlace of PublicationContributorsLocation
Done
Filters
Reset
50,312
result(s) for
"Hemophilia"
Sort by:
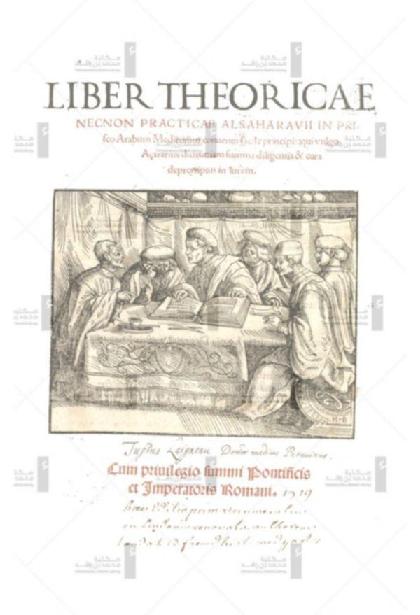
Liber theoricae necnon practicae Alsaharavii : in prisco Arabum medicorum conventu facile principis
by
الزهراوي، خلف بن عباس، توفي 1036 author
,
Burgkmair, Hans, 1473-1531 contributor
,
Ricius, Paulus, 1480-1541 contributor
in
Medicine, Arab
,
Hemophilia Early works to 1800
,
Hemophilia
1519
\"The first two books of al Zahrāwī's systematic treatise on medicine entitled al Tasrif; translated from the Arabic. Edited by P. Ricius.\"--Brit. Mus. Gen. cat. 1962. v. 122, col. 751.
Rare Book
Haemophilia
2025
Haemophilia A and B are congenital X-linked bleeding disorders resulting from deficiencies in clotting factors VIII (haemophilia A) and IX (haemophilia B). Patients with severe deficiency, defined as having less than 1% of normal plasma factor activivity, often have spontaneous bleeding within the first few years of life. Those with moderate and mild deficiencies typically present with post-traumatic or post-surgical bleeding later in life. A high index of suspicion and measurement of factor activity in plasma facilitates early diagnosis. In the 21st century, therapeutic advances and comprehensive care have substantially improved both mortality and morbidity associated with these conditions. Management strategies for haemophilia include on-demand treatment for bleeding episodes and all surgeries and regular treatment (ie, prophylaxis) aimed at reducing bleeds, morbidity, and mortality, thereby enhancing quality of life. Treatment options include factor replacement therapy, non-replacement therapies that increase thrombin generation, and gene therapies that facilitate in vivo clotting factor synthesis. The therapies differ in their use for prophylaxis and on-demand treatment, the mode and frequency of administration, duration of treatment effect, degree of haemostatic protection, and side-effects. Monitoring the effectiveness of these prophylactic therapies involves assessing annual bleeding rates and joint damage. Personalised management strategies, which align treatment with individual goals (eg, playing competitive sports), initiated at diagnosis and maintained throughout the lifespan, are crucial for optimal outcomes. These strategies are facilitated by a multidisciplinary team and supported by clinician-led education for both clinicians and patients.
Journal Article
Liber theoricae necnon practicae Alsaharavii : in prisco Arabum medicorum conventu facile principis
by
الزهراوي، خلف بن عباس، توفي 1036 author
,
Burgkmair, Hans, 1473-1531 contributor
,
Ricius, Paulus, 1480-1541 contributor
in
Latin language Texts
,
Medicine, Arab
,
Hemophilia Early works to 1800
1519
\"The first two books of al Zahrāwī's systematic treatise on medicine entitled al Tasrif; translated from the Arabic. Edited by P. Ricius.\"--Brit. Mus. Gen. cat. 1962. v. 122, col. 751.
Rare Book
A Leap Forward in Hemophilia A Treatment
2024
Efanesoctocog alfa, a novel factor VIII replacement therapy, emerges as one of the options for improved prophylaxis in pediatric patients with hemophilia A.
Journal Article
The past and future of haemophilia: diagnosis, treatments, and its complications
by
Garagiola, Isabella
,
Young, Guy
,
Peyvandi, Flora
in
Antibodies, Neutralizing - immunology
,
Clinical trials
,
Coagulants - immunology
2016
Haemophilia A and B are hereditary haemorrhagic disorders characterised by deficiency or dysfunction of coagulation protein factors VIII and IX, respectively. Recurrent joint and muscle bleeds lead to severe and progressive musculoskeletal damage. Existing treatment relies on replacement therapy with clotting factors, either at the time of bleeding (ie, on demand) or as part of a prophylactic schedule. The major complication of such therapy is the development of neutralising antibodies (ie, inhibitors), which is most frequent in haemophilia A. Treatment might improve considerably with the availability of new modified drugs, which might overcome existing prophylaxis limitations by reducing dosing frequency and thereby rendering therapy less distressing for the patient. Subcutaneous administration of some new therapies would also simplify prophylaxis in children with poor venous access. Gene therapy has the potential for a definitive cure, and important results have been obtained in haemophilia B. Despite improvements in haemophilia care, the availability of clotting factor concentrates for all affected individuals worldwide remains the biggest challenge.
Journal Article
C57 CRITICAL CARE CASE REPORTS: HEMATOLOGY, ONCOLOGY, RHEUMATOLOGY, AND IMMUNOLOGY: The Case Of The Curtailed Clotting Cascade
2017
Introduction: While many coagulopathies can be managed on the medical ward, it is the intensive care unit that often comes face to face with severe and life-threatening clotting impairments. Unfortunately, her condition worsened necessitating an ICU transfer upon developing acute respiratory distress syndrome and hemoptysis thought to be from pulmonary alveolar hemorrhage.
Journal Article
C57 CRITICAL CARE CASE REPORTS: HEMATOLOGY, ONCOLOGY, RHEUMATOLOGY, AND IMMUNOLOGY: Double Trouble: Bullous Pemphigoid And Acquired Factor Viii Inhibitor In A Rapidly Decompensating Patient
2017
Due to concern of a causative association between phenytoin and both the patient's bullous pemphigoid and acquired factor VIII inhibitor, the antiepileptic was discontinued. Conclusion: Cases of factor VIII inhibitor are relatively rare but life-threatening, and are often associated with malignancies and auto-immune diseases.
Journal Article
Gene Therapy for Hemophilia
by
Davidoff, Andrew M.
,
Nienhuis, Arthur W.
,
Nathwani, Amit C.
in
Animal models
,
Bleeding
,
Blood Transfusion
2017
The X-linked bleeding disorder hemophilia causes frequent and exaggerated bleeding that can be life-threatening if untreated. Conventional therapy requires frequent intravenous infusions of the missing coagulation protein (factor VIII [FVIII] for hemophilia A and factor IX [FIX] for hemophilia B). However, a lasting cure through gene therapy has long been sought. After a series of successes in small and large animal models, this goal has finally been achieved in humans by in vivo gene transfer to the liver using adeno-associated viral (AAV) vectors. In fact, multiple recent clinical trials have shown therapeutic, and in some cases curative, expression. At the same time, cellular immune responses against the virus have emerged as an obstacle in humans, potentially resulting in loss of expression. Transient immune suppression protocols have been developed to blunt these responses. Here, we provide an overview of the clinical development of AAV gene transfer for hemophilia, as well as an outlook on future directions.
Several successful studies of AAV-mediated, liver-targeted transfer of genes encoding clotting factors FIX and FVIII are ongoing for patients with severe hemophilia B and A, respectively. The early results of these studies and the critical questions that remain to be answered are discussed in this review.
Journal Article
Treatment patterns and bleeding outcomes in persons with severe hemophilia A and B in a real-world setting
2020
The current standard of care treatment for severe hemophilia A and B (SHA and SHB) is the prophylactic intravenous replacement of coagulation factor VIII or IX (FVIII/FIX) to prevent spontaneous bleeding. Persons with hemophilia without prophylactic treatment receive therapy in case of bleeding, i.e., on demand. To assess treatment patterns, utilization of products, and bleeding outcomes in a real-world cohort of persons with SHA and SHB, defined as FVIII or FIX activity < 1%, data was retrospectively collected from hemophilia-specific patient diaries used for home treatment, medical records, and entries into the Austrian Hemophilia Registry from the year 2012 to 2017. Fifty-three male persons with SHA (n = 47) and SHB (n = 6) were included; 26 with SHA and 5 with SHB were on prophylaxis, 8 and 1 switched therapy regimen, and 13 and 0 received on-demand therapy. Persons on prophylaxis used a mean factor FVIII or FIX dose of 71.7 and 40.1 IU/kg/week. Median (IQR) annualized bleeding rates (ABR) in SHA were 28.0 (23.4–31.3) in the on-demand, 4.9 (1.6–13.5) in the prophylaxis group, and 3.0 (2.0–6.8) in the prophylactic group of SHB. Three persons with SHA had zero bleeds during the observation period. On-demand therapy and hepatitis B and C were associated with higher ABR but not age, weight, and HIV positivity. Bleeding rates and the proportion of on-demand therapy in persons with hemophilia were high in our real-world cohort. Further improvement is needed, which might be facilitated with the advent of factor products with extended half-life or non-factor therapies.
Journal Article
Differences in Major Bleeding Events Between Patients With SevereHemophilia A and Hemophilia B: A Nationwide, Population-Based CohortStudy
2019
There has been an ongoing debate as to whether hemophilia A (HA) ismore severe than hemophilia B (HB), and there are studiessupporting each side of the argument. The study aimed to investigate whether anydifferences in major bleeding events exist between patients with severe HA andHB. A nationwide, population-based retrospective cohort study using the NationalHealth Insurance Research Database was conducted. We compared 658 patients withsevere HA and 137 patients with severe HB without inhibitors from 1997 to 2013,during the period when adult patients older than 18 years old were treated withthe on-demand therapy since birth. There was no significant difference betweenpatients with severe HA and HB in the rate of major bleeding events, with anadjusted relative ratio of 0.79 (95% confidence interval [CI]:0.36-1.71, P = .548). There was also nosignificant difference in the incidence rate of major bleeding events betweenadult patients with HA and HB with the on-demand therapy, and an adjusted hazardratio (HR) of 0.82 (95% CI: 0.65-1.02).However, patients with HA had a lower incidence rate of intracranial hemorrhage,with an adjusted HR of 0.44 (95% CI: 0.25-0.79). Inaddition, no significant difference in the frequency of major bleeding eventsrequiring hospitalization between patients with HA and HB was found,P > .05. In conclusion, the study demonstrated thatpatients with severe HB encountered a similar rate of major bleeding events tothose with severe HA.
Journal Article