Catalogue Search | MBRL
Search Results Heading
Explore the vast range of titles available.
MBRLSearchResults
-
DisciplineDiscipline
-
Is Peer ReviewedIs Peer Reviewed
-
Reading LevelReading Level
-
Content TypeContent Type
-
YearFrom:-To:
-
More FiltersMore FiltersItem TypeIs Full-Text AvailableSubjectCountry Of PublicationPublisherSourceTarget AudienceDonorLanguagePlace of PublicationContributorsLocation
Done
Filters
Reset
566,356
result(s) for
"LIVER"
Sort by:
Phase 3 Trial of Semaglutide in Metabolic Dysfunction–Associated Steatohepatitis
2025
Semaglutide, a glucagon-like peptide-1 receptor agonist, is a candidate for the treatment of metabolic dysfunction-associated steatohepatitis (MASH).
In this ongoing phase 3, multicenter, randomized, double-blind, placebo-controlled trial, we assigned 1197 patients with biopsy-defined MASH and fibrosis stage 2 or 3 in a 2:1 ratio to receive once-weekly subcutaneous semaglutide at a dose of 2.4 mg or placebo for 240 weeks. The results of a planned interim analysis conducted at week 72 involving the first 800 patients are reported here (part 1). The primary end points for part 1 were the resolution of steatohepatitis without worsening of liver fibrosis and reduction in liver fibrosis without worsening of steatohepatitis.
Resolution of steatohepatitis without worsening of fibrosis occurred in 62.9% of the 534 patients in the semaglutide group and in 34.3% of the 266 patients in the placebo group (estimated difference, 28.7 percentage points; 95% confidence interval [CI], 21.1 to 36.2; P<0.001). A reduction in liver fibrosis without worsening of steatohepatitis was reported in 36.8% of the patients in the semaglutide group and in 22.4% of those in the placebo group (estimated difference, 14.4 percentage points; 95% CI, 7.5 to 21.3; P<0.001). Results for the three secondary outcomes that were included in the plan to adjust for multiple testing were as follows: combined resolution of steatohepatitis and reduction in liver fibrosis was reported in 32.7% of the patients in the semaglutide group and in 16.1% of those in the placebo group (estimated difference, 16.5 percentage points; 95% CI, 10.2 to 22.8; P<0.001). The mean change in body weight was -10.5% with semaglutide and -2.0% with placebo (estimated difference, -8.5 percentage points; 95% CI, -9.6 to -7.4; P<0.001). Mean changes in bodily pain scores did not differ significantly between the two groups. Gastrointestinal adverse events were more common in the semaglutide group.
In patients with MASH and moderate or advanced liver fibrosis, once-weekly semaglutide at a dose of 2.4 mg improved liver histologic results. (Funded by Novo Nordisk; ClinicalTrials.gov number, NCT04822181.).
Journal Article
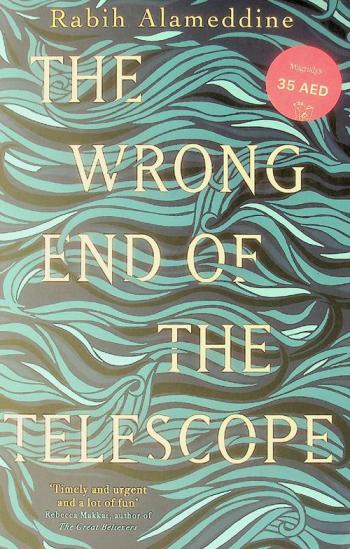
The wrong end of the telescope
Mina Simpson, a Lebanese doctor, arrives at the infamous Moria refugee camp on Lesbos, Greece, after being urgently summoned for help by her friend who runs an NGO there. Alienated from her family except for her beloved brother, Mina has avoided being so close to her homeland for decades. But with a week off work and apart from her wife of thirty years, Mina hopes to accomplish something meaningful, among the abundance of Western volunteers who pose for selfies with beached dinghies and the camp's children. Soon, a boat crosses bringing Sumaiya, a fiercely resolute Syrian matriarch with terminal liver cancer. Determined to protect her children and husband at all costs, Sumaiya refuses to alert her family to her diagnosis. Bonded together by Sumaiya's secret, a deep connection sparks between the two women, and as Mina prepares a course of treatment with the limited resources on hand, she confronts the circumstances of the migrants' displacement, as well as her own constraints in helping them.
A Phase 3, Randomized, Controlled Trial of Resmetirom in NASH with Liver Fibrosis
2024
Resmetirom is a selective agonist of THR-β. In adults with nonalcoholic steatohepatitis and fibrosis, daily resmetirom (80 mg or 100 mg) was superior to placebo with respect to NASH resolution and fibrosis improvement.
Journal Article
Efruxifermin in Compensated Liver Cirrhosis Caused by MASH
by
Patil, Rashmee
,
Rinella, Mary E.
,
de Temple, Brittany
in
Aged
,
Antifibrotic Agents - administration & dosage
,
Antifibrotic Agents - adverse effects
2025
In phase 2 trials involving patients with stage 2 or 3 fibrosis caused by metabolic dysfunction-associated steatohepatitis (MASH), efruxifermin, a bivalent fibroblast growth factor 21 (FGF21) analogue, reduced fibrosis and resolved MASH. Data are needed on the efficacy and safety of efruxifermin in patients with compensated cirrhosis (stage 4 fibrosis) caused by MASH.
In this phase 2b, randomized, placebo-controlled, double-blind trial, we assigned patients with MASH who had biopsy-confirmed compensated cirrhosis (stage 4 fibrosis) to receive subcutaneous efruxifermin (at a dose of 28 mg or 50 mg once weekly) or placebo. The primary outcome was a reduction of at least one stage of fibrosis without worsening of MASH at week 36. Secondary outcomes included the same criterion at week 96.
A total of 181 patients underwent randomization and received at least one dose of efruxifermin or placebo. Of these patients, liver biopsy was performed in 154 patients at 36 weeks and in 134 patients at 96 weeks. At 36 weeks, a reduction in fibrosis without worsening of MASH occurred in 8 of 61 patients (13%) in the placebo group, in 10 of 57 patients (18%) in the 28-mg efruxifermin group (difference from placebo after adjustment for stratification factors, 3 percentage points; 95% confidence interval [CI], -11 to 17; P = 0.62), and in 12 of 63 patients (19%) in the 50-mg efruxifermin group (difference from placebo, 4 percentage points; 95% CI, -10 to 18; P = 0.52). At week 96, a reduction in fibrosis without worsening of MASH occurred in 7 of 61 patients (11%) in the placebo group, in 12 of 57 patients (21%) in the 28-mg efruxifermin group (difference from placebo, 10 percentage points; 95% CI, -4 to 24), and in 18 of 63 patients (29%) in the 50-mg efruxifermin group (difference from placebo, 16 percentage points; 95% CI, 2 to 30). Gastrointestinal adverse events were more common with efruxifermin; most events were mild or moderate.
In patients with compensated cirrhosis caused by MASH, efruxifermin did not significantly reduce fibrosis at 36 weeks. (Funded by Akero Therapeutics; SYMMETRY ClinicalTrials.gov number, NCT05039450.).
Journal Article
Resmetirom (MGL-3196) for the treatment of non-alcoholic steatohepatitis: a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial
by
Bashir, Mustafa R
,
Bansal, Meena B
,
Harrison, Stephen A
in
Adult
,
Alanine Transaminase - blood
,
Biomarkers
2019
Non-alcoholic steatohepatitis (NASH) is characterised by hepatic steatosis, inflammation, hepatocellular injury, and progressive liver fibrosis. Resmetirom (MGL-3196) is a liver-directed, orally active, selective thyroid hormone receptor-β agonist designed to improve NASH by increasing hepatic fat metabolism and reducing lipotoxicity. We aimed to assess the safety and efficacy of resmetirom in patients with NASH.
MGL-3196-05 was a 36-week randomised, double-blind, placebo-controlled study at 25 centres in the USA. Adults with biopsy confirmed NASH (fibrosis stages 1–3) and hepatic fat fraction of at least 10% at baseline when assessed by MRI-proton density fat fraction (MRI-PDFF) were eligible. Patients were randomly assigned 2:1 by a computer-based system to receive resmetirom 80 mg or matching placebo, orally once a day. Serial hepatic fat measurements were obtained at weeks 12 and 36, and a second liver biopsy was obtained at week 36. The primary endpoint was relative change in MRI-PDFF assessed hepatic fat compared with placebo at week 12 in patients who had both a baseline and week 12 MRI-PDFF. This trial is registered with ClinicalTrials.gov, number NCT02912260.
348 patients were screened and 84 were randomly assigned to resmetirom and 41 to placebo at 18 sites in the USA. Resmetirom-treated patients (n=78) showed a relative reduction of hepatic fat compared with placebo (n=38) at week 12 (−32·9% resmetirom vs −10·4% placebo; least squares mean difference −22·5%, 95% CI −32·9 to −12·2; p<0·0001) and week 36 (−37·3% resmetirom [n=74] vs −8·5 placebo [n=34]; −28·8%, −42·0 to −15·7; p<0·0001). Adverse events were mostly mild or moderate and were balanced between groups, except for a higher incidence of transient mild diarrhoea and nausea with resmetirom.
Resmetirom treatment resulted in significant reduction in hepatic fat after 12 weeks and 36 weeks of treatment in patients with NASH. Further studies of resmetirom will allow assessment of safety and effectiveness of resmetirom in a larger number of patients with NASH with the possibility of documenting associations between histological effects and changes in non-invasive markers and imaging.
Madrigal Pharmaceuticals.
Journal Article
A Placebo-Controlled Trial of Subcutaneous Semaglutide in Nonalcoholic Steatohepatitis
2021
Patients with nonalcoholic steatohepatitis were randomly assigned to receive subcutaneous semaglutide or placebo. The incidence of NASH resolution was significantly higher with semaglutide than with placebo, but the between-group difference in the incidence of an improvement in fibrosis stage was not significant.
Journal Article
FIB-4 as a screening and disease monitoring method in pre-fibrotic stages of metabolic dysfunction-associated fatty liver disease (MASLD)
by
Albert, Stewart G.
,
Wood, Emily M.
in
Adult
,
Alanine Transaminase - blood
,
Aspartate Aminotransferases - blood
2024
Guidelines emphasize screening high-risk patients for metabolic dysfunction-associated steatotic liver disease (MASLD) with a calculated FIB-4 score for therapy to reverse fibrosis. We aimed to determine whether FIB-4 can effectively screen and monitor changes in steatohepatitis (MASH).
Data were retrieved from the NIDDK-CR R4R central repository, of the CRN/PIVENS (pioglitazone vs vitamin E vs placebo) trial of adult patients without diabetes mellitus and with MASLD.
220 patients with MASLD had alanine transaminase (ALT), aspartate aminotransferase (AST) and platelet count, to calculate FIB-4, and repeat liver biopsies for histological MASLD activity scores (NAS). Compared to NAS score of 2, Fib-4 was higher at NAS 5) (p = 0.03), and NAS score of 6 (p = 0.02). FIB-4 correlated with cellular ballooning (r = 0.309, p < 0.001). Levels of ALT (ANOVA, p = 0.016) and AST (ANOVA p = 0.0008) were associated with NAS. NAS improved with pioglitazone by 39 %, p < 0.001 and with vitamin E by 36 %, p < 0.001. Pioglitazone and vitamin E both improved histological sub-scores for steatosis, and inflammation, without statistical changes in fibrosis grade. Changes in FIB-4 correlated with changes in NAS (r = 0.237, p < 0.001).
In this post hoc analysis, changes in FIB-4 were associated with changes of steatohepatitis. Medication known to treat steatohepatitis, may be considered, before the onset of advanced fibrosis.
•FIB-4 is used in metabolic dysfunction-associated steatotic liver disease (MASLD) to screen for fibrosis.•A post hoc review of the NIDDK-CR R4R central repository of CRN/PIVENS trial evaluated FIB-4 in pre-fibrotic steatohepatitis.•Changes in FIB-4 correlated with changes in histological steatohepatitis.•Therapies with pioglitazone and Vitamin E improved inflammation by 37 %–35 % without changes in fibrosis.•Medication known to treat steatohepatitis, may be considered, before the onset of advanced fibrosis
Journal Article
A Phase 2 Randomized Trial of Survodutide in MASH and Fibrosis
2024
In this phase 2 trial involving adults with metabolic dysfunction–associated steatohepatitis and liver fibrosis, survodutide was superior to placebo with respect to improvement in MASH without worsening of fibrosis.
Journal Article
The effects of resveratrol supplementation on cardiovascular risk factors in patients with non-alcoholic fatty liver disease: a randomised, double-blind, placebo-controlled study
by
Adibi, Payman
,
Hekmatdoost, Azita
,
Faghihzadeh, Forouzan
in
Adult
,
alanine transaminase
,
Alanine Transaminase - blood
2015
Non-alcoholic fatty liver disease (NAFLD) is usually associated with insulin resistance, central obesity, reduced glucose tolerance, type 2 diabetes mellitus and hypertriacylglycerolaemia. The beneficial effects of resveratrol on metabolic disorders have been shown previously. The aim of this study was to evaluate the effects of resveratrol supplementation on cardiovascular risk factors in patients with NAFLD. In this randomised double-blinded placebo-controlled clinical trial, fifty NAFLD patients were supplemented with either a 500-mg resveratrol capsule or a placebo capsule for 12 weeks. Both groups were advised to follow an energy-balanced diet and physical activity recommendations. resveratrol supplementation reduced alanine aminotransferase (ALT) and hepatic steatosis significantly more than placebo (P<0·05). BMI, waist circumference, serum aspartate aminotransferase, bilirubin, HDL-cholesterol and apo a1 were reduced significantly in both groups (P<0·05); however, there were no significant differences between the two groups (P>0·05). There were no significant changes in blood pressure, insulin resistance markers and TAG in either group (P>0·05). Our data have shown that 12-week supplementation of 500 mg resveratrol does not have any beneficial effect on anthropometric measurements, insulin resistance markers, lipid profile and blood pressure; however, it reduced ALT and hepatic steatosis in patients with NAFLD.
Journal Article